In a recent article featured in the scientific journal Nature Metabolism, a group of scientists embarked on an extensive, long-term investigation. They meticulously examined and analyzed the lipidome by studying plasma samples collected from more than a hundred individuals for a duration of nine years. This comprehensive study aimed to unravel the significance of different lipid categories in the context of human health, the aging process, and the development of various diseases.
Background
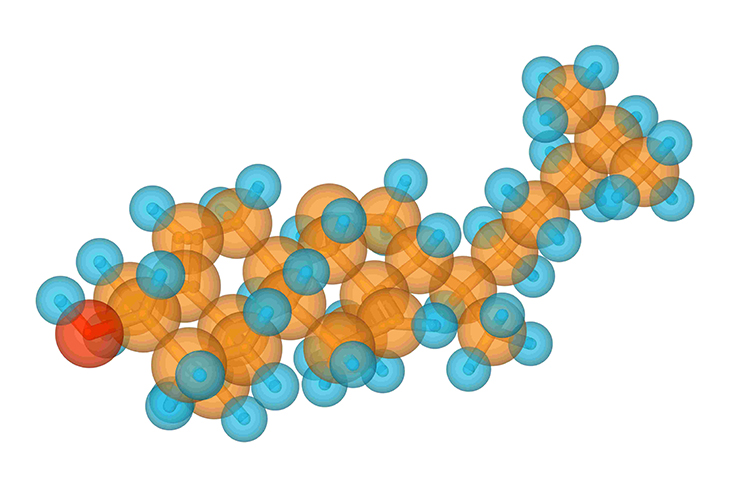
Lipids serve indispensable functions within the human body, contributing to vital processes like cell signaling, the maintenance of cellular structures, and energy regulation. They can originate from either external sources or internal processes, existing in various forms and sizes. These lipid categories include triacylglycerols, phosphatidylethanolamines, cholesterol esters, lysophosphatidylcholines, ceramides, and lysophosphatidylethanolamines. Despite the pivotal roles they play in human physiology, there remains a shortage of information regarding how lipids change in individuals over time and in relation to diseases.
The advancement of high-throughput omics technologies has revolutionized our ability to investigate human physiology and comprehend the alterations that occur in the molecular landscape during disease progression. However, while next-generation sequencing and innovative mass spectrometry methods have made genomics and proteomics research more accessible and cost-effective, the intricate diversity of metabolites in the body has posed challenges for understanding metabolomics. Lipids represent a substantial portion of the metabolome and play a crucial role in modulating inflammatory processes. This underscores the importance of comprehending longitudinal changes in the lipidome to gain insights into the pathophysiology of diseases.
About the study
In this current study, the researchers conducted an extensive analysis of lipid profiles in a cohort of more than 100 participants over a nine-year period. They employed a highly precise and rapid mass spectrometry technique to comprehensively quantify various lipids. Plasma samples were collected from the participant group, which included individuals with both insulin resistance and sensitivity, at ten different time points during this nine-year span.
The collection of plasma samples followed a specific schedule: every three months when participants were in good health and three to seven times within a three-week period during periods of illness. Additionally, alongside lipid profiling, various clinical laboratory parameters were assessed for each sample. Moreover, given that samples were obtained during times of illness or stress, the researchers also conducted profiling of 62 chemokines, cytokines, and growth factors.
To perform the lipid profiling, the researchers employed a quantitative, high-throughput lipidomic process that utilized a triple-quadrupole mass spectrometer and a differential mobility separation device. This innovative method allowed for the quantification and identification of more than a thousand lipids, spanning 16 different subclasses such as lysophosphatidylcholines, free fatty acids, triacylglycerides, diacylglycerols, and various types of ceramides.
The study initially characterized the baseline lipidome using 802 samples from 96 participants who were free of acute diseases at the study’s outset. Furthermore, the researchers investigated those lipid subclasses that exhibited the greatest variability among participants, seeking to understand the extent to which these variations were attributable to individual differences. The research also delved into the relationship between the overall lipidome profile derived from the healthy baseline measurements and other clinical parameters. For lipids that displayed a negative correlation with clinical measures, the researchers explored potential associations between these lipids and the microbiome.
Results
The research findings unveiled associations among aging, insulin resistance, and viral respiratory infections, highlighting dynamic shifts in the lipidome. These observations underscored the crucial role of lipids in regulating inflammation and maintaining immune system balance. Notably, individuals with insulin resistance exhibited disruptions in immune homeostasis, alongside alterations in clinical markers’ relationships with lipids and accelerated changes in various lipid subclasses during the aging process.
The study further elucidated that distinct biological functions are attributed to specific lipid subclasses, revealing that conventional clinical lipid profiles often lack the precision needed to comprehend metabolic health. The outcomes also demonstrated a correlation between ester-linked phosphatidylethanolamines, which possess antioxidant properties and participate in cell signaling, and favorable traits marked by elevated high-density lipoprotein levels and reduced steady-state plasma glucose.
Moreover, the research uncovered a decline in ester-linked phosphatidylethanolamine levels during the early stages of infection, contributing to heightened inflammation. Additionally, phosphatidylethanolamines exhibited associations with insulin resistance or sensitivity, as well as age and gender-related patterns.
Conclusions
In this extensive and thorough longitudinal examination of the lipidome, conducted on a substantial sample size, we have uncovered compelling evidence highlighting the pivotal role that lipids play in both maintaining health and contributing to the development of diseases. These findings underscore the significance of lipids as not only essential components of our physiological makeup but also as valuable indicators and potential targets for preventive and therapeutic interventions.
The research has illuminated how the intricate landscape of lipids within our bodies can serve as valuable biomarkers, providing crucial insights into an individual’s health status and susceptibility to various conditions. By monitoring changes in lipid profiles, clinicians and researchers can gain valuable information about a person’s overall well-being and their risk of developing specific diseases. This, in turn, opens up new avenues for early detection and intervention, potentially improving health outcomes.
Moreover, the study has unveiled a particularly noteworthy aspect of lipidomics – the age and sex-specific signatures exhibited by distinct lipid subclasses. These unique signatures suggest that tailoring therapeutic strategies based on an individual’s age and gender may be essential for optimizing treatment effectiveness. By recognizing these differences, healthcare providers can develop personalized approaches that better address the specific needs and vulnerabilities of their patients, ultimately enhancing the quality of care and treatment outcomes.
Hence, this comprehensive longitudinal analysis of the lipidome underscores the multifaceted role of lipids in our health and disease processes. It not only positions lipids as vital indicators and targets for medical interventions but also emphasizes the importance of considering age and sex-specific variations in lipid profiles when designing preventive and therapeutic strategies. This research holds the promise of advancing personalized medicine, where treatments are tailored to each individual’s unique lipidomic profile, ultimately leading to more effective and targeted healthcare.



