Physician-scientists at the University of Pittsburgh have pioneered an AI-powered application aimed at mitigating unnecessary antibiotic prescriptions for children by enabling the diagnosis of ear infections through a smartphone interface.
The prospect of misdiagnosing an ear infection in a child, coupled with the inadvertent administration of superfluous antibiotics, poses a significant concern. Such antibiotics can wreak havoc on the delicate gut microbiome during critical developmental stages.
Statistics reveal that roughly 70% of children encounter an ear infection before reaching the age of one, with acute otitis media (AOM) being the most prevalent form. Nonetheless, distinguishing AOM from other conditions like fluid buildup behind the ear often proves challenging, resulting in misdiagnoses and inappropriate treatment protocols.
Dr. Alejandro Hoberman, the study’s lead author and a distinguished professor of pediatrics, elucidates the repercussions of such diagnostic errors. Underdiagnosing AOM leads to inadequate medical attention, while its overdiagnosis prompts unnecessary antibiotic prescriptions, thereby compromising the efficacy of available antibiotic treatments.
To address this pressing issue, Dr. Hoberman and his research team embarked on a groundbreaking endeavor. They curated and meticulously annotated a comprehensive training dataset comprising 1,151 videos showcasing the tympanic membrane (commonly known as the eardrum) from pediatric patients. These videos were sourced from 635 children who sought medical care at outpatient pediatric facilities affiliated with the University of Pittsburgh Medical Center spanning the period from 2018 to 2023.
By leveraging this extensive dataset, the AI tool developed by the research team promises to revolutionize the diagnosis of ear infections, thereby ensuring more accurate and efficient medical interventions for pediatric patients.
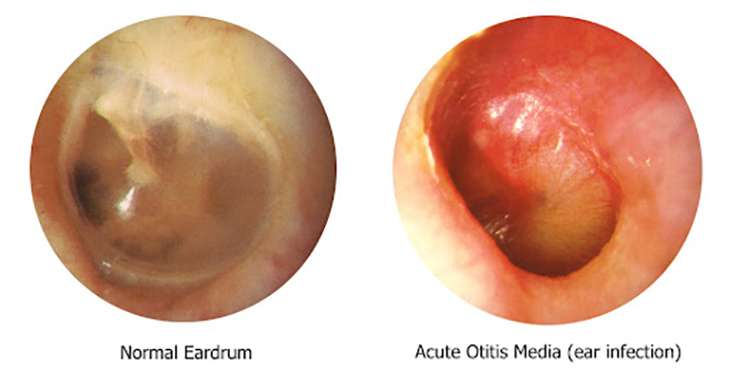
“The eardrum is a thin, flat piece of tissue that stretches across the ear canal,” Dr. Hoberman elaborated. “In AOM, the eardrum bulges like a bagel, leaving a central area of depression that resembles a bagel hole.”
“In contrast, in children with otitis media with effusion, no bulging of the tympanic membrane is present.”
Two seasoned specialists, possessing substantial expertise in Acute Otitis Media (AOM) research, meticulously reviewed the provided videos, discerning whether each case presented signs of AOM or not. Subsequently, the research team leveraged these diagnoses to train two distinct artificial intelligence (AI) models.
The finalized AI tool operates by analyzing video footage capturing the eardrum of a patient. It scrutinizes various attributes such as shape, position, color, and translucency of the eardrum to render a diagnostic assessment.
The outcomes, disseminated in the esteemed journal JAMA Pediatrics, unveiled a commendable diagnostic accuracy of 93%. Additionally, the tool demonstrated minimal instances of both false negatives and false positives.
Comparatively, previous investigations involving clinicians have showcased varying diagnostic accuracies for AOM, ranging from 30% to 84%. These variances were contingent upon factors such as the type of healthcare provider, their level of training, and the age of the pediatric patient under evaluation.
“These findings suggest that our tool is more accurate than many clinicians,” Dr. Hoberman stated. “It could be a game-changer in primary health care settings to support clinicians in stringently diagnosing AOM and guiding treatment decisions.”
He further mentioned that another advantage of the tool lies in its ability to diagnose by analyzing a brief video of the eardrum taken with an otoscope connected to a mobile phone camera. Additionally, these videos can be stored and utilized for enhancing diagnostic accuracy in the future.
“The videos we capture can be stored in a patient’s medical record and shared with other providers, meaning we can show parents and/or students what we see and explain why we are or are not making a diagnosis of ear infection,” he also said.
“It is important both as a teaching tool and for reassuring parents that their child is receiving appropriate treatment.”
Hoberman is optimistic that the recently developed technology will soon see widespread the implementation across healthcare facilities.



