A new study published on March 20 in JAMA found that a simple skin biopsy test conducted at the doctor’s office can detect Parkinson’s disease with 93 percent accuracy.
This special biopsy, known as the Syn-One Test, has previously shown effectiveness in identifying various neurological disorders. However, this study was the first to focus on a subgroup of a neurodegenerative conditions collectively known as synucleinopathies.
These conditions include Parkinson’s disease, Lewy body dementia, multiple system atrophy, and pure autonomic failure. The study was conducted in a large, blinded fashion across multiple centers in the United States.
Lead author Christopher Gibbons, MD, a neurologist at Beth Israel Deaconess Medical Center and a professor of neurology at Harvard Medical School in Boston, says, “Too often patients experience delays in diagnosis or are misdiagnosed due to the complexity of these diseases.”
Dr. Gibbons notes that the ability to detect the abnormal protein associated with Parkinson’s disease and related conditions with such high accuracy will lead to better diagnostic outcomes and improved care for patients.
More Than 1 in 4 Patients Receive Incorrect Diagnosis Before Parkinson’s Diagnosis
According to the authors, an estimated 180,000 people in the United States are diagnosed with Parkinson’s disease, Lewy body dementia, and related disorders each year. Despite Parkinson’s disease being the most well-known of the synucleinopathies, Lewy body dementia is actually more common.
However, because these conditions share overlapping signs and symptoms such as tremors and cognitive changes, diagnosis can be challenging. A 2020 survey conducted by Parkinson’s UK revealed that 1 in 4 people reported being misdiagnosed with a different condition before receiving the correct Parkinson’s diagnosis.
Lewy body dementia can also be misdiagnosed because its cognitive symptoms, especially early in the disease course, can resemble those of Alzheimer’s disease. It is crucial to distinguish between the two because some medications used for Alzheimer’s symptoms can cause serious side effects in people with Lewy body dementia.
Test Accurately Identified Individuals with Neurodegenerative Diseases in 93 to 100 Percent of Cases
Researchers from 30 academic and community-based neurology practices across the United States recruited 428 participants aged between 40 and 99. Among them were 151 healthy individual without brain disease and 277 individuals diagnosed with one of the four neurodegenerative diseases, confirmed by physical examination and symptoms assessment by an expert panel.
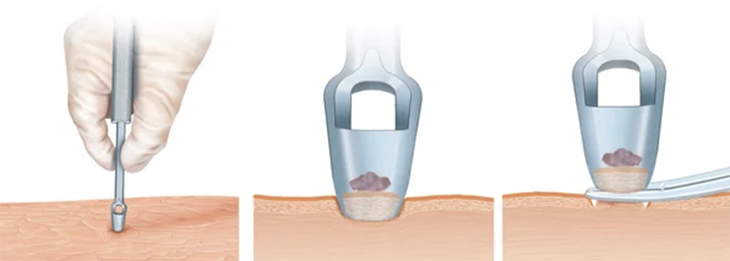
Participants underwent three 3-millimeter skin punch biopsies, taken from the neck, knee, and ankle. The researchers were specifically searching for an abnormal protein called phosphorylated alpha-synuclein (P-SYN), which is commonly observed in the brain and spinal cord of individuals with synucleinopathies.
According to the study, these were the key findings:
- In people with clinically confirmed Parkinson’s disease, 93 percent demonstrated a positive skin biopsy for P-SYN that confirmed the diagnosis.
- Participants with Lewy body dementia and multiple system atrophy tested positive 96 percent and 98 percent of the time, respectively.
- A full 100 percent of people with pure autonomic failure were positive for the abnormal protein.
In the control group, slightly over 3 percent of individuals had biopsies that tested positive for P-SYN. The authors suspect this error rate may indicate that some of the healthy controls are at risk for one of the conditions, as the protein can be present in the skin even in the earliest stages of the diseases.
According to Rizwan Akhtar, MD, PhD, as assistant professor of neurology at Northwestern Medicine in Chicago, the fact that almost no skin samples from health individuals showed aggregates of P-SYN, while the vast majority of samples from patients did, suggests that the skin might offer a window to observe what is happening in the brain.
How Does a Basic Skin Biopsy Detect Brain Disease?
Dr. Akhtar explains that many neurodegenerative diseases are believed to result from the formation of protein clumps inside and around brain cells, which disrupt cell function.
Since these clumps cannot be directly observed in the living brain, many scientists are working to identify biomarkers that could indicate the presence of the disease in other parts of the body or fluids. Although not directly involved in this study, Dr. Akhtar oversees several clinical trials focused on finding biomarkers of neurodegenerative diseases in body fluids.
The groundwork for this breakthrough was laid in 2009 when researchers discovered that Parkinson’s disease affects peripheral nerves, including those outside the brain and spinal cord, such as those in the skin. These nerves are associated with many non-motor symptoms of the disease, such as constipation and issues with blood pressure control or urination.
Researchers hypothesized that P-SYN might also be present in the peripheral nerves in the skin.
Skin Biopsy Test May Aid in Developing Improved Treatments
The test not only improves diagnosis and treatment but also holds promise for advancing treatments for these diseases.
Developing new treatments for conditions like Parkinson’s disease is extremely challenging. Using the test to identify individuals early in the disease course before they enroll in trials can confirm their diagnosis of one of the four diseases.
Currently, the biopsy test cannot differentiate between these conditions. However, there is hope that it can be refined over time to do so, according to Dr. Akhtar.
“In addition, being able to measure the amount of protein in the nerves is critical if you are hoping that a new therapy is going to be able to reduce this protein,” says Gibbons.
Researchers hope to repeat the test over time to monitor changes in the amount of this protein, but it has not been confirmed whether the test can predict disease progression.
Who Should Consider the Skin Test for Parkinson’s Disease and Other Neurogenerative Diseases?
According to Dr. Gibbons, the Syn-One Test has been available since 202, and it is currently being used by over 1,000 neurologists across the United States.
Dr. Gibbons says, “In general, this test is most useful to help clarify a particular diagnosis — for example, does a person have Parkinson’s disease or is this parkinsonism induced by a medication.” In that example, the latter would not possess the abnormal protein.
“It can be used for people who have symptoms that are not exactly diagnostic for Parkinson’s disease, where the physician is not sure. We are doing two additional studies that look at much earlier stages of disease to see if we can make a diagnosis before all the symptoms are present, and we anticipate those results over the next year or so,” says Dr. Gibbons.
Notably, several of the authors have stock in the company that manufactures the tests, CND Life Sciences.