Is there a link between inflammation and anxiety? Experts have asked this question for years. In their research, they have noticed growing evidence that the two may be linked. While there is still much to learn about the relationship, the medical cases reported may be worth looking into.
Anxiety is something that millions of people go through. When faced with a stressful situation, the trepidation becomes evident every now and then. Then, there are those who suffer from anxiety disorder. They experience anxiety more frequently. The feelings are also lot more intense and happen more persistently.
For these sufferers, the emotions don’t come at will. When it hits them, they find that the emotions they have are extremely difficult to control to the point that it becomes disruptive as they try to live as normally as possible.
Types of Anxiety Disorders
When it comes to anxiety disorders, there are ranges involved. Among which are:
- Generalized nxiety disorder (GAD)
- Social anxiety disorder, which is also referred to as social phobia
- Separation anxiety disorder
- Post-traumatic stress disorder (PTSD)
It’s good to also note that some sufferers experience more than one form of anxiety disorder at the same time, which makes it even more difficult for them.
According to the World Health Organization, anxiety disorders are common. In 2015, an estimated 3.6 percent of the global population suffered from an anxiety disorder. This amounts to roughly 264 million folks from all four corners of the globe.
Possible Causes
Scientists and health experts still cannot be certain about precise causes of anxiety. However, they have come up with a few likely factors such as the following:
- an overactivity in certain parts of the brain
- An imbalance of neurotransmitters
- Genetics
- Trauma
- Personality traits
- Chronic pain
- Substance misuse
Even before the pandemic plagued the world, the number of anxiety sufferers have slowly been increasing. The numbers are even more prominent in the West. Hence, it is imperative that people understand how and why anxiety disorders emerge. There are hardworking scientists who have been doing nonstop work when it comes to investigating the potential role of inflammation in triggering anxiety.

Definition of Inflammation
Inflammation is basically man’s natural and beneficial reaction to harmful stimuli. A few examples of which are irritants or pathogens. This is actually protective response that allows the body to defend and protect itself by getting rid of the offending stimuli. While this may be a protective response, long-term inflammation can also damage the cells and tissues it had protected to begin with.
Inflammation also occurs in different parts of the body, even the brain. And as mentioned, while inflammation may have protective benefits, researchers are interested to see whether or not chronic inflammation could influence and encourage the development of mental disorders.
Inflammation and Anxiety
Although there is substantial evidence of the link between inflammation and depression, not too much research has been conducted on the connection between inflammation and anxiety. Those who have studied it, however, are starting to build a solid body of evidence.
Anxiety disorders are characterized by mental distress. Those who suffer from it are also more prone to of coronary heart disease, atherosclerosis, and metabolic disorders.
The abovementioned conditions involve low grade systemic inflammation. Doctors have also discovered that since depression often comes hand in hand with anxiety, they are now hypothesizing that inflammation might actually play a role in anxiety.
Signs of Inflammation
The scientists behind the study on inflammation have focused on key markers present in the body. Markers honed in on are C-reactive protein (CRP), interleukin-6 (IL-6), and tumor-necrosis factor (TNF)-alpha.
CRP is released from the liver as a response to inflammation. Its main role is to bind to markers on dead or dying cells or microorganisms. Health experts believe that by binding to its target, CRP aids the complement system, which, in turn, strengthens the ability of immune cells to clear away the pathogens and dead cells.
IL-6 and TNF-alpha, on the other hand, are both cytokines that promote the inflammation that happens. Cytokines are a broad category of proteins that play a vital role in the communication between cells.
The Evidence Gathered
Over the years of study, the evidence gathered on links between anxiety and inflammation have strengthened. In one study, for instance, scientists evaluated a range of inflammation and coagulation markers. These markers included CRP, IL-6, and TNF-alpha in 853 participants. The researchers gathered a group of volunteers and asked them to fill out a 40-item questionnaire to look into how anxious they felt at that very moment. Then, the questions broadened to how anxious they are generally. They gathered the findings and these showed that higher anxiety scores were associated with increased levels of CRP, IL-6, and TNF-alpha in men, and higher levels of CRP and IL-6 in women.
In the Journal of Psychiatric Research, a study investigated the connection between inflammation and PTSD. The researchers behind it compared pro-inflammatory markers in 14 people with PTSD with those of 14 people without the condition. The study may not have included a larger set of participants, but they were able to conclude that “PTSD patients showed a low grade systemic pro-inflammatory state, which, moreover, was related to PTSD symptom levels […].” A review on PTSD and inflammation states that PTSD is associated with increased IL-6, TNF-alpha, and other markers of inflammation.
The researchers have also looked into women living with both type 2 diabetes and phobic anxiety, and another study found a link between inflammatory markers and anxiety. The authors behind these say, “High levels of phobic anxiety are associated with increased levels of leptin and inflammatory markers.”
Leptin is a hormone that helps control regulate appetite. It is in charge of caloric intake. However, scientists believe that leptin plays a crucial part in chronic inflammation.
A systematic review and meta-analysis, published in Depression & Anxiety, looked deep into the large data gathered from 41 related and important studies. The researchers came to a conclusion and said, “These data demonstrate the association between inflammatory dysregulation and diagnoses associated with chronic, impactful, and severe anxiety and [provide] insight into the way that anxiety, and in particular PTSD, is related to certain inflammatory markers.”
Triggering Inflammation Experimentally
While researchers have seen how people with anxiety are more likely to experience inflammation. It does not necessarily work the other way around. There is no proof that inflammation causes or increases the risk of anxiety.
This has always been a question asked. The “which-came-first-the-chicken-or-the-egg type of question forces experts to ask whether inducing a state of inflammation would increase the chances of a person to suffer from anxiety. Hence, they triggered inflammation by injecting the study’s participants with lipopolysaccharide (LPS), a component of the cell membrane of gram-negative bacteria, to induce an inflammatory response.
They found that as the inflammatory markers increased, so did anxiety. They also saw that those whose IL-6 levels increased also experienced the highest anxiety levels. While it is extremely difficult to translate animal studies on mental health to the human experience, research conducted in mice saw worthy results. One study, in fact, saw the scientists induce gastrointestinal inflammation in mice. They found that the rodents developed anxiety-like behavior. They also observed that Bifidobacterium longum, a probiotic bacterium, reversed the changes made. So, what did this mean? Which brings us to understanding more about microbiomes.
Microbiome Role
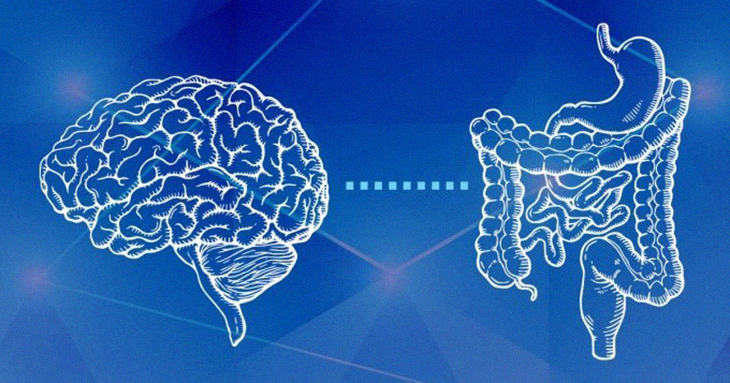
As scientists have delved deeper into the link between the immune system and the brain, some are more interested on the important role for gut bacteria. It was a few years ago the idea of how bacteria in our gut could influence mental health sounded ludicrous. Today, however, opinions have changed. The gut, as they say, is the body’s second brain because it has a highly complex nervous system, which experts refer to as the enteric nervous system.
Recent studies suggest that the gut could actually be considered the first brain. Why? Because evolutionarily speaking, it was there before the brain found in our skills. There is a complex two-way communication and relationship between the enteric nervous system and the central nervous system. These two communicate regularly, and as the authors of one paper say, “Insights into the gut-brain cross talk have revealed a complex communication system that not only ensures the proper maintenance of gastrointestinal homeostasis but it is likely to have multiple effects on affect, motivation, and higher cognitive functions.”
Gut bacteria has direct access to the brain by way of the enteric nervous system. In fact, some research show links between anxiety and changes in gut bacteria populations. In fact, one found “decreased microbial richness and diversity” in people with GAD when they compared these with to those without anxiety. Probiotic foods contain live microorganisms, and prebiotics are nondigestible ingredients that encourage bacterial growth.
One meta-analysis collated data from different studies. As a matter of fact, they looked at 34 research materials. These studies looked into the impact of prebiotics and probiotics on depression and anxiety. Overall, researchers found that there is effect from prebiotics. However, they also said, “Probiotics yielded a small but significant effects for depression and anxiety.”
While multiple mechanisms are most likely involved, gut bacteria might actually influence levels of anxiety through inflammation. That’s because bacterial found in the gut have tight connections to the nervous system. These also interact with the immune system, the very thing that drives the inflammatory response. Still, while gut bacteria may seem like something worth studying more, there is yet so much to learn about these.
Cause or Effect?
So, does inflammation cause or aggravate anxiety? Does anxiety promote inflammation? Does reducing inflammation ease symptoms? There are no answers yet at this time, but there are clues. An example would be one study that focused on cancer patients. After patients received their diagnosis, they had increased risk of psychiatric disorders as well. This study included 316,904 people cancer sufferers.
The scientists again gathered and collected information about which participants developed mental disorders and whether or not they were ingesting aspirin, a nonsteroidal anti-inflammatory drug (NSAIDs). Those who had NSAIDs during the year before diagnosis showed, “Pre-diagnostic use of aspirin was associated with a decreased risk of depression, anxiety, and stress-related disorders during the first year following cancer diagnosis.”
However, similar researches have not had the same findings.
The Bottomline
Although there is more solid evidence in link between inflammation and mental health, scientists have a long road ahead of them. They need time before they can fully understand the relationship between anxiety and inflammation. Why? Because the immune system is complicated and dynamic. Moreover, mental health have not been fully explained even at this point. Microbiome are also extremely complex. Put these all together, and the scientists have a lot to unpack.
Still, they haven’t given up home. These researchers and scientists are trying to slowly chip away the mysterious in order to get a clearer picture. For now, it does seem likely that inflammation plays some role.