Clinicians have claimed that depression and heart disease can sometimes have overlapping symptoms, which may confuse the person suffering from one of either.
Those who suffer from depression are extremely aware of how this condition hurts the heart. The emotional pain takes its toll eventually, but not too many are aware of how feeling depressed can take affect the heart and vice versa.
The relationship between the two is a two-way street. Why? How? First of all, depression increases the risk of heart issues by as much as 64 percent,. This may sound too steep but this is according to the National Heart, Lung, and Blood Institute. Moreover, they say that about one in five folks with heart disease experience major depression.
So, how exactly are feeling depression and heart health related? Here are four ways by which depression intertwines with your heart health, as stated by the experts in the field.
1. Depression Increases Risk of Suffering from Cardiovascular Disease
“Depression is a well-known risk factor for cardiovascular disease, not just because of its psychological impact but also from the physiological standpoint,” Rashmi Parmar, MD, said. He is an adult and child psychiatrist with Mindpath Health in Newark, California.
Cardiovascular disease is a group of disorders that affect both the heart and blood vessels. This is known to be the number-one killer in the United States alone. Experts say that this is often a silent killer as well. This was reported by the Centers for Disease Control and Prevention (CDC).
Heart disease is a type of cardiovascular disease. This is oftentimes already precipitated by a condition known as atherosclerosis, as stated by American Heart Association. Much research has been done on this and findings show how those who suffer from depression have an increased risk of atherosclerosis-related cardiovascular disease. A large study was published in June 2019 in BMJ Open. This showed how people ages 40 to 80 and who suffer from depression have an increased risk of atherosclerosis-related cardiovascular disease.
As for atherosclerosis, this affects blood vessels known as the arteries. These arteries are responsible for transporting oxygen-rich blood from the heart to the rest of the body. Over time and as you get older, these arteries gradually stiffen, and as a result, plaque accumulates along its walls. Many of those with atherosclerosis don’t experience the symptoms that are already there, especially those with mild cases. In some cases, on the other hand, arterial stiffness and plaque buildup make it hard for blood to flow normally through these arteries. This increases risk of a heart attack or stroke, both cases can potentially be fatal for those who suffer from it.
2. Depression Lowers the Chances of You Making Heart-Healthy Lifestyle Choices
Here’s a fact: depression makes it difficult to even get out of bed. Hence, chances are that you won’t exercise and cook nutritious meals for yourself during these days. People who are depressed are prone to unhealthy eating habits. More importantly, they don’t get enough exercise, which may explain the weight gain at times. Some also resort to smoking. These facts were shared by Arvind Nirula, MD, an interventional cardiologist at MemorialCare Heart and Vascular Institute at Orange Coast Medical Center in Fountain Valley, California. He said, “These are all risk factors for hypertension, diabetes, high cholesterol, and heart disease itself.”
3. Depression May Stop You From Getting Help for Heart Symptoms
Those who have been diagnosed with depression can experience a heart-related symptom such as rapid heartbeat or chest pain. These signs, as well as the thought that they may need to deal with a serious health diagnosis, can be scary. Even those who don’t suffer from depression are hesitant about this. Can you imagine what it must be like for those who are? This could be overwhelming for them, and making an appointment with a doctor to discuss these symptoms is just too much to handle.
“People with depressive symptoms may not have the energy or motivation to follow up with medical appointments,” said Ernesto Lira de la Rosa, PhD. He is a licensed clinical psychologist based in New York City and a media adviser for the Hope for Depression Research Foundation. Still, it’s very vital to see a doctor to have these new symptoms checked. That’s because depression and heart issues share symptoms at times. One that can be attributed to depression may actually have another underlying cause. For instance, “Depression and heart disease often have overlapping symptoms such as fatigue and anxiety,” said Rigved Tadwalkar, MD. He is a cardiologist at Providence Saint John’s Health Center in Santa Monica, California.
“For this reason, patients with these symptoms, along with symptoms and risk factors for heart disease, should be evaluated in a timely manner by their physician,” Dr. Tadwalkar said as he advised those with the condition to have themselves checked.
4. Depression Sometimes Follows a New Heart Diagnosis and Can Even Make Exacerbate It
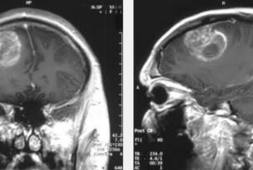
For those who have recently suffered from a heart attack, or had a heart surgery, or have been diagnosed with a heart condition such as coronary artery disease (which is a buildup of plaque in the main arteries of the heart), this can sometimes lead to depression after, as according to the Cleveland Clinic.
“Having a heart health condition may mean more doctor’s appointments, lifestyle changes, medication to manage the condition, and increased stress of having to adapt to a new way of life,” Dr. Lira de la Rosa said. De la Rosa also added, “This can be overwhelming and lead some individuals to develop depressive symptoms.”
If this will not be treated, depression can make an existing heart condition worse and increase the risk of a heart attack. The Cleveland Clinic states warns against this because untreated depression is especially risky for the older individuals who have coronary artery disease. Studies were published in August 2016 in the journal BMC Psychiatry.