In a new study, researchers are looking at the link between high blood pressure and epilepsy. What they found is that high blood pressure does increase the risk of epilepsy by around 2.5 times, but when patients take antihypertensive medications, it lessens the risk.
What they found is that although high blood pressure does increase the risk factor for epilepsy, more research is required to better understand the fundamental association between the two.
According to the NCBI website, ‘epilepsy is the third most common neurological disorder affecting older adults after stroke and dementia, and the incidence of epilepsy is increasing rapidly in this population.’
Moreover, other research has also found that late-onset epilepsy has become more widespread over the past two decades. If the numbers continue to rise as the aging population also increases, then epilepsy could possibly become a public epidemic in the years to come.
Regardless, the underlying cause in 32 to 48% of all cases of epilepsy is still largely unclear. But according to some research, it’s the vascular risk factors that could lead to the risk of late-onset epilepsy. Meanwhile, other studies show that these vascular risk factors that are involved in epilepsy can begin in someone who is only in their 30s.
By better understanding the role that vascular risk factors play in late-onset epilepsy can definitely aid in the way policymakers create public health measures, as well as preventive strategies to help hamper and manage the rising rates of this condition.
Just recently, researchers from the Boston University School of Medicine located in the United States conducted a study that examined the link between vascular risk factors and the onset of epilepsy.
What they discovered was that ‘hypertension had links to an almost 2-fold higher risk of developing late-onset epilepsy.’ And for those that didn’t use any medication to regulate their blood pressure, the risk was even higher.
You can see the study in Epilepsia.
Looking at the Data Analysis
The research group took data from the Framingham Heart Study (FHS), which is an ongoing, community-based study that started way back in 1948. Since then, it’s Offspring Cohort follows the health outcomes of the health examinations done every four years of 5,124 children of the original participants.
For the study, the researchers took data from 2,986 participants who went to their fifth examination between the years 1991 and 1995, that were at least 45 years old within those years, and those that had health records that showed data on vascular risk factors.
Such vascular risk factors that were collected ‘included systolic and diastolic blood pressure.’ The study authors also characterized ‘high blood pressure as systolic blood pressure of 140 millimeters of mercury (mmHg) and above, and diastolic blood pressure of 90 mm Hg and above, as well as the use of antihypertensive medications.
They also screened for the following health conditions in the participants, such as body mass index (BMI), cholesterol levels, smoking status, diabetes, cardiovascular disease and stroke.
To properly screen participants for issues of epilepsy or seizure, the research group ‘sued routine chart reviews for neurological conditions, self-reported seizures, International Classification of Diseases Ninth Revision (ICD-9) codes linked to epilepsy or seizures, and antiepileptic drug use.’
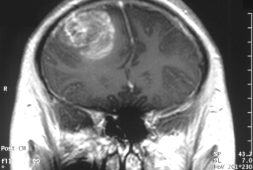
Researchers also looked at brain imaging and electroencephalography (EEG), cardiac and other relevant data to establish the cases of epilepsy in participants.
Within the study group, the researchers also found 55 examples of epilepsy, where ’26 were definite, 15 probable, and 14 suspected.’ The individuals’ involved had an average age of 73.8 years old at the time of their potential diagnosis.
Moreover, researchers discovered that hypertension had associations to an almost 2-fold higher risk of epilepsy, although there were no links to epilepsy to the other risk factors.
After removing those participants that took antihypertensive meds, the researchers also noted that high blood pressure was associated withs a 2.44-fold higher risk of developing epilepsy. Researchers also found that ‘every 10 mm Hg change in systolic blood pressure was associated with a 17% higher risk of developing epilepsy.’
Looking At the Underlying Mechanisms
There are a number of theories that could possibly explain the association between hypertension and epilepsy. One of these mechanisms could be due to the renin-angiotensin system, which regulates blood pressure.
Research done in rats shows that after they had repetitive seizures, they have ‘2.6 – 8.2 times the components of RAS than mice without seizures. Antihypertensive drugs that lowered levels of RAS components delayed seizure onset and reduced seizure frequency.’
But like most studies, more research is needed to better understand just how much this mechanism explains the link between hypertension and epilepsy, while other research implies that the system could have a limited effect.
The researchers also explain that another possible underlying mechanism could be a small vessel disease (SVD), which is a condition wherein the walls of the small arteries and capillaries are damaged, which means they can’t deliver sufficient oxygen-rich blood to all the organs. In a recent study, the scientists discovered that ‘the duration of high blood pressure is a strong predictor of SVD in later life.’
The research group also adds that SVD is associated to temporal lobe epilepsy. Likely mechanisms also include ‘cortical microinfarcts, small lesions in cortical tissue, and the disruption of U fibers that may lead to excessive excitability and thus seizures. U fibers connect neighboring areas of the cerebral cortex.’
In conclusion, the researchers share that hypertension is truly an independent predictor of late-onset epilepsy which carries a 2-fold risk of developing seizures after 45 years or more.
The Limitations
The study authors also share that their study has limitations, of course. While it primarily included white participants, it didn’t necessarily represent all races and ethnicities. The researchers also share that since the study’s nature is an observational one, it means that it’s cannot prove causality.’
According to Dr. Jason Hauptman, who happens to be a neurosurgeon at Seattle Children’s Hospital, explained to Medical News Today (MNT), “These results are particularly interesting because whether or not high blood pressure (hypertension) in and of itself is an independent risk factor for stroke has been a topic of controversy. The thought is that independent of the presence of stroke, hypertension may lead to disease of small arteries throughout the brain that can cause injuries on the microscopic level.”
He added, “These injuries could potentially lead to epilepsy with or without the presence of a visible or symptomatic stroke. This research is important because hypertension is not only common, but it is modifiable – that is, we may have ways of assessing and treating it. This would need to be pursued in larger, more diverse patient populations to fully assess exactly how much this is a risk factor and to test the potential interventions.”
Meanwhile, cardiologist at Mayo Clinic Healthcare in London, Sanjay Prasad, M.D., who was not involved with the study was asked by MNT whether he found the results surprising. He shared that they weren’t surprising and actually match former study findings.
He said, “This work is observational, so does not confirm that there is a definite direct link. However, it builds on our knowledge base and highlights the importance of lifestyle, regular exercise, and a low salt intake to control blood pressure as an important way of reducing morbidity.”
“[These results highlight] the need for aggressive control of blood pressure – and encourage everyone – particularly those above the age of 50, to regularly monitor their blood pressure. We also need to assess the impact of blood pressure control in those with epilepsy and after a stroke.”