Scientists Formulate Drug For Type 1 Diabetes That Has Ability To Protect Cells Within The Pancreas

Scientists at Johns Hopkins University have announced promising results from an experimental antibody drug, mAb43, which appears to prevent and even reverse the onset of type 1 diabetes in mice. This breakthrough also extends the lifespan of the treated mice.
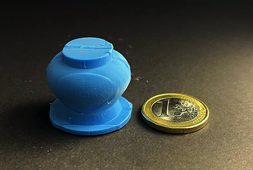
mAb43 is unique in its approach. It specifically targets insulin-producing beta cells in the pancreas, protecting them from the body’s immune system, which mistakenly attacks these cells in type 1 diabetes. This targeted action suggests that mAb43 could be used long-term in humans with minimal side effects. Monoclonal antibodies like mAb43 are produced by cloning, which involves creating identical replicas of a single cell line.
The findings, detailed in the May issue of Diabetes, offer hope for a new treatment for type 1 diabetes. This autoimmune condition affects about 2 million Americans, including both children and adults, and currently has no cure or preventative measures. In type 1 diabetes, the immune system destroys the pancreatic cells that produce insulin, unlike type 2 diabetes where the pancreas produces insufficient insulin.
Dr. Dax Fu, an associate professor of physiology at Johns Hopkins and the leader of the research team, explains that mAb43 binds to a specific protein on the surface of beta cells. These cells are located in clusters known as islets within the pancreas. The drug essentially cloaks the beta cells, hiding them from the immune system’s destructive attacks.
In their study, the researchers administered a weekly dose of mAb43 to 64 non-obese mice, genetically predisposed to develop type 1 diabetes, starting when they were 10 weeks old. After 35 weeks of treatment, none of the mice developed diabetes, demonstrating the drug’s efficacy.
While these results are promising, the current version of the antibody is designed for mice. The next step for the researchers is to develop a humanized version of mAb43 for future studies and potential clinical use.
In five of the same type of diabetes-prone mice, the researchers denied the rodents from getting the weekly mAb43 doses until the reached14 weeks old, and then continued to give these dosages while being monitored until they were 75 weeks old. “One of the five in the group developed diabetes, but no adverse events were found,” the researchers said.
When mAb43 was administered early in the study, the treated mice exhibited significantly extended lifespans, surviving for the entire monitoring period of over 75 weeks. In stark contrast, the control group of mice that did not receive mAb43 only survived for 18 to 40 weeks.
The researchers, partially funded by the National Institutes of Health, then conducted a more detailed examination of the treated mice. They used a biological marker known as Ki67 to determine whether beta cells in the pancreas were multiplying. The findings were encouraging: after treatment with mAb43, immune cells withdrew from the vicinity of the beta cells, leading to a marked reduction in inflammation. This retreat of immune cells allowed the beta cells to begin reproducing slowly, indicating a restoration of the pancreatic function.
These results suggest that mAb43 not only protects existing beta cells from immune system attacks but also promotes the regeneration of these critical insulin-producing cells. This dual action enhances the potential of mAb43 as a transformative treatment for type 1 diabetes.
“mAb43 in combination with insulin therapy may have the potential to gradually reduce insulin use while beta cells regenerate, ultimately eliminating the need to use insulin supplementation for glycemic control,” team member and postdoctoral fellow Devi Kasinathan said.
The research team discovered that mAb43 binds specifically to beta cells, which constitute approximately 1% to 2% of the cells in the pancreas. This targeted binding is crucial for the drug’s effectiveness in protecting these insulin-producing cells from immune system attacks.
In a related development, another monoclonal antibody drug, teplizumab, received approval from the U.S. Food and Drug Administration in 2022. Teplizumab operates differently from mAb43; it binds to T cells, modulating their activity to make them less harmful to beta cells. This drug has demonstrated the ability to delay the onset of clinical (stage 3) type 1 diabetes by about two years. This delay is particularly beneficial for young children diagnosed with the disease, providing them additional time to mature and learn how to manage the necessary lifelong insulin injections and dietary restrictions.
Both mAb43 and teplizumab represent significant advancements in the treatment and management of type 1 diabetes. While teplizumab delays disease onset by targeting the immune system’s T cells, mAb43 directly protects and promotes the regeneration of beta cells. These complementary approaches offer hope for improved quality of life and disease outcomes for individuals with type 1 diabetes.
“It’s possible that mAb43 could be used for longer than teplizumab and delay diabetes onset for a much longer time, potentially for as long as it’s administered,” Fu said.
The Hopkins researchers are actively working to develop a humanized version of the mAb43 antibody. Their next steps include conducting clinical trials to evaluate its safety, identify potential side effects, and assess its effectiveness in preventing type 1 diabetes in humans.