Multiple Sclerosis (MS) is an often-misunderstood condition. Hence, to start the MS month, it may be time to fully understand it by knowing what it is, what it does, and the common misconceptions about it.
What is MS?
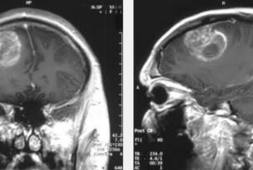
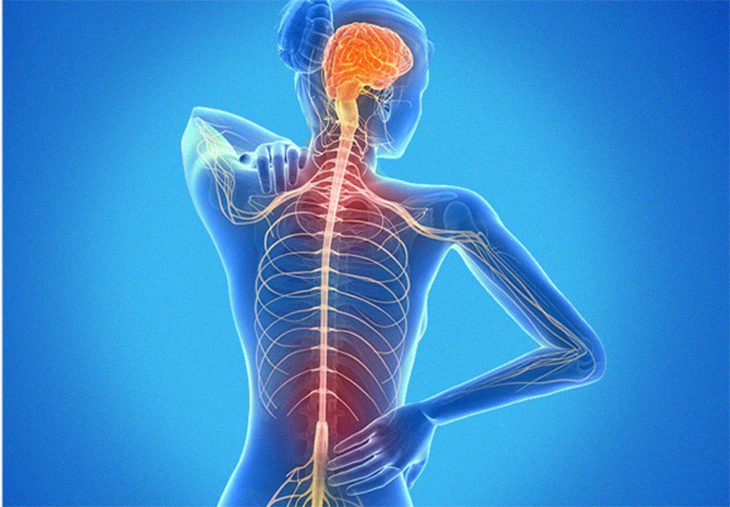
To start with, multiple sclerosis is a chronic disease. It affects both the brain and the spinal cord. This is a lifelong disease that may eventually lead to neurological disabilities. It comes with several symptoms and is immune-mediated. In fact, doctors consider this to be an autoimmune disease.
The disease attacks the myelin, the protective substance covering the nerve fibers. Hence, complications in the body arise since it attacks the brain. As a result, signals between the brain and the rest of the body can no longer work in proper tandem. The communication between the two loses efficacy.
A study in 2016 also found that over 2.2 million were affected by MS.
The multiple of symptoms affects any part of the body and includes the following:
- Numbness and tingling
- Vision issues
- Muscle spasms and weakness
- Fatigue
- Anxiety and depression
- Pain
- Mobility problems
- Difficulty talking
- Trouble with swallowing
Some of those affected by MS sees the disease intensify after a certain amount of time. Doctors call this condition primary progressive MS. Others, however, experience “attacks” as it worsens. During the latter, the symptoms either become worse or new ones are felt. This called relapsing-remitting MS.
For some, relapsing-remitting MS gradually worsens over time and this condition is called secondary progressive MS.
At this point in time, it is still unclear why some people develop MS. Health experts believe that environmental and genetic factors play a vital part. But because there is no definitive answer as to why MS occurs, many have bought into several myths.
The Nine Common MS Myths
For your proper education, we will elucidate the nine most common myths and misconceptions that often go with MS:
Myth 1: Everyone with MS eventually will need to use a wheelchair.
This is clearly a myth. The MS Society, in fact, explains, “Most people with MS don’t use a wheelchair.”
Fifteen years after patients are diagnosed, only 20 of them need a form of walking aid, be it a wheelchair, a crutch, or a cane when walking.
Dr. Loren A. Rolak, a neurologist, reports her findings in a research paper. The MS Society also says, “If your MS does start to affect your mobility, the decision to start using a walking stick, mobility scooter, or wheelchair can be a difficult one. But once you start using one, you may find — as many people with MS do — how useful they are and how they can help you to retain your independence.”
Myth 2: People with MS lose the ability to hold down a job.
Again, another myth. MS sufferers can become extremely valuable members of the workforce. While they do face unusual challenges and may even need to change careers, this doesn’t happen to everyone. The National Multiple Sclerosis Society wrote in their report, “People living with MS often continue working long after their diagnosis.”
The MS Society also says, “Some people with MS decide to leave their jobs when they are first diagnosed or experience their first major exacerbation, often at the suggestion of their family or doctor.” However, some of the sufferers are quick to make that decision “at a time when symptoms can color judgment. Disease-modifying therapies, new technologies, better symptom management, legal employment protections, and community resources can help you remain in the workforce.”
Regular work may even be beneficial to many as one study explains: “In addition to providing financial security, employment can contribute significantly to the physical and mental wellbeing of the people with MS, providing a source of support and interaction, and a sense of identity and purpose.”
Myth 3: Only the older group of individuals develop MS.
In reality, people with MS have started seeing signs when they were between 20 to 40 years of age. So, MS can appear any time. There are no age specifications. In fact, it’s very rare for many to develop MS at 50 years old.
However, as the authors of a study explain that distinguishing late-onset MS from other conditions associated with advancing age can be difficult. So developing MS may be more common than what experts have estimated.
Myth 4: People with MS are not allowed to exercise.
This is far from the truth because exercise can actually help with symptoms. Working on the muscles improves balance and enhances strength. Out of all the myths, this one is the most pervasive. As the researchers behind coping suggestions say, some people suffering from MS often automatically lead sedentary lives because they fear that the symptoms could worsen. However, the experts behind this study recommend, “Exercise should be considered as a safe and effective means of rehabilitation in MS patients. Existing evidence shows that a supervised and individualized exercise program may improve fitness, functional capacity, and quality of life, as well as modifiable impairments in MS patients.”
The National Multiple Sclerosis Society collaborated with experts of the area and published a comprehensive guide to the exercises highly recommended. Among their claims, they elaborate, ”Healthcare providers should encourage at least 150 minutes each week of exercises and/or at least 150 minutes each week of lifestyle and physical activity. […] Progress toward these targets should be gradual, based on the person’s abilities, preferences, and safety.”
Ultimately, however, It is important to consult with a doctor before getting into a regimen.
Myth 5: There is no need for medication of symptoms are minor.
Treatment is a must at all times. During the early phases of MS, the symptoms may be mild, which can make people assume that they can dismiss these. It is important to note that early treatment and long-term follow-up can actually slow down its progression. A study published in 2016 investigated the effects of early intervention and concluded that “early treatment initiation was associated with a better clinical outcome.”
Myth 6: Women with MS should never plan a pregnancy.
The Multiple Sclerosis has spoken about this, and the experts say, “A pregnancy is not automatically high risk just because the mother has MS. […] If you have MS, you are no more likely to experience a miscarriage or birth abnormalities in your baby than a woman who does not have MS.” The disease does not hinder your efforts nor does it cause issues during pregnancy.
People with relapsing-remitting MS are less likely to experience a relapse during the none months. In fact, the risk of a relapse increases six months after childbirth. In 2019, the Association of British Neurologists published a consensus on guidelines. They covered the things that needed to be done pre-pregnancy to actual birth. They recommend counseling and advice from experts instead. They also recognized that “having MS does not affect fertility or risk of miscarriage,” and that “pregnancy does not increase the risk of worsening long-term disability.” And all throughout pregnancy, the authors recommended that patients “should not defer disease-modifying drug treatment because they wish to have children in the future.”
Myth 7: MS is passed on from parent to child.
MS does have a genetic component to it, but it is not passed directly from parent to child. It occurs unpredictably. Several studies have proven this to be true when they studied identical twins. If one develops MS, there is a 20 to 40 percent chance that the other twin will, too. In nonidentical twins, the risk lowers to 3 to 5 percent.
So while genetics are involved, there is more to MS than meets the eye. So far, scientists have discovered and pointed out more than 200 gene regions that contribute to MS susceptibility. According to the studies made by MS Society, 1 in 67 children who have a parent with MS develop the same autoimmune disease. This is compared with a roughly 1 in 500 risk for those who do not have MS in their family.
Hence, while the risk factors are higher, inheriting MS is note foregone assumption.
Myth 8: People with MS must avoid stress and anxiety at all cost.
Stress is a part of life, that is true, and while highly emotional events can exacerbate the symptoms and that patients are more likely to become anxious, life’s curveballs cannot be avoided.
Rather, it is better to find ways for better stress management. more effectively. As the authors of a brochure produced by the National Multiple Sclerosis Society say, “Stress can’t be – and shouldn’t be – totally avoided. The challenge is to reduce its intensity and us it to work for, not against, us.”
Another similar myth states that stressful life events might increase the risk of developing MS. There is zero evidence for this.
Myth 9: MS is a fatal disease.
Although MS is an autoimmune lifelong struggle. That much is true, but is not fatal, and it should never be assumed that this is the case.
According to one study, MS reduces a person’s lifespan by roughly 7 years. This very same study also found that “survival was shortest in the earliest birth cohort for both populations.” From this, the average lifespan may actually be gradually increasing, given that the patient gets the proper help. Thanks to the hardworking scientists and health experts who have investigated this disease, researched tirelessly about it, and developed new treatments, MS should not greatly affect the sufferer’s life and his/her lifespan.