Most people with asthma use either inhaled or oral glucocorticoids. But a new study suggests that these type of drugs has been associated with structural changes within the brain which has gone on to explain the psychological and neurological side effects observed with these medications.
Lead study author, Merel van der Meulen of the Leiden University Medical Center in the Netherlands wrote in the journal BMJ Open published last August 30, “This study shows that both systemic and inhaled glucocorticoids are associated with an apparently widespread reduction in white matter integrity.”
Around half of the tissue in the brain is made up of white matter, and it’s main job is to transmit messages between the brain and the rest of the body. There is a link between reduced white matter volume and cognitive decline, especially when it comes to attention, processing information, and memory loss. Moreover, decreased white matter has also been associated with a number of mental health issues, such as anxiety, depression, and bipolar disorder.
While glucocorticoids have previously been linked to damaging changes in the brain, and even mood disorders and cognitive decline, a lot of the former research has shown mixed results since they were based on animal studies or human trials that were too small to support bigger conclusions.
As for the new study, the research team looked at data from the UK BioBank, which happens to be a large-scale biomedical database and research resource that has genetic and health information on at least half a million adults. This new analysis utilized data from cognitive and psychological assessments, brain scans, and prescription records for ‘222 patients who used oral glucocorticoids, 557 individuals who used inhaled glucocorticoids, and a control group of 24,106 people who didn’t use these drugs.’
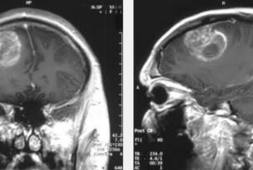
However, none of the participants they included in the study had a history of any neurological, psychological, or hormonal disorders. In addition, none of the participants took antidepressants or other medication for mood disorders. They did have completed cognitive testing, brain magnetic resonance imaging (MRI) scans, and answered questionnaires to identify which symptoms of mood disorders.
When these were compared with people that had never used glucocorticoids, what researchers found was those that did use these types of drugs had significantly more damage to their white matter in the brain, as well as greater reductions in their white matter volume.
The study also found that the biggest damage was seen in those using oral glucocorticoid users who were made to take these medications for longer periods of time. Since oral drugs are systemic medicines – which means they travel all throughout the body – they tend to have more profound side effects than inhaled steroids, which target the airways.
When it came to the results of the assessments of processing speed in oral glucocorticoid users, they had significantly worse cognitive test scores as compared to the people in the control group. Oral glucocorticoid users also showed substantially more psychological symptoms, like apathy and depression.
As for inhaled glucocorticoids, the study also found that these drugs seemed to have much lower impact on cognitive performance, brain structure, and psychological symptoms than the oral version of these medications.
Notably, glucocorticoids are often prescribed to treat a number of medical conditions, such as asthma, rheumatoid arthritis, inflammatory bowel disease (IBD), and some autoimmune diseases like lupus and particular cancers.
As for rescue inhalers used for asthma, they don’t actually use glucocorticoids. Rather, these quick-acting inhalers contain drugs known as bronchodilators that help to open airways and relax the muscles in the lungs. As for patients with poorly controlled asthma or have severe asthma may be told to use oral or inhaled glucocorticoids in order to better manage the inflammation that occurs from the disease that can also exacerbate the symptoms of asthma.
Looking at the limitations of the new study, one in particular is that researchers lacked data on the exact dose of glucocorticoids prescribed to patients. Another limitation is that the prescription data also lacked information on how often people actually took their medications as directed by their doctor. Moreover, the study was not a controlled experiment ‘described to prove whether or how glucocorticoids might directly cause damaging changes in the brain.’
Research assistant professor at the Michigan Neuroscience Institute in Ann Arbor, Joanna Spencer-Segal, MD, PhD, who was not part of the new study, said, “We can’t draw definitive conclusions about whether glucocorticoids caused the observed changes in brain structure and function that were seen in systemic and inhaled glucocorticoid users.”
But, it is possible that as observed in the study, the changes seen in the brain were really because of the glucocorticoids. Dr. Spencer-Segal shares, “Systemic glucocorticoids are known to cause serious side effects, especially if taken for a long time.”
There are many cases where doctors can treat patients without have to use these types of drugs.
“People who take glucocorticoids should talk to their doctor about whether glucocorticoids might be decreased or discontinued. Do not stop taking glucocorticoids without consulting your doctor, since stopping them abruptly can be dangerous,” Dr. Spencer-Segal adds.
As for Thomas Ritz, PhD, professor and director of the Psychobiology of Stress, Emotion, and Chronic Disease Research Program at Southern Methodist University in Dallas, who also was not part of the study, said that asthmas patients in particular need to prioritize their symptoms properly.
Dr. Ritz explains, “We’ve known for a long time that we should avoid systemic corticosteroids as much as possible, as long as asthma is not severe. Inhaled corticosteroids have been the mainstay for regular ‘maintenance’ treatment of asthma for some time now. The key here is to find for patients the lowest possible dose that controls their asthma well.”