New Study By Scientists Find Relief For Treatment-Resistant Depression By Locating Target For Deep Brain Stimulation

Researchers at the University of Texas Health-Houston conducted a very small study on just 10 patients, but they were able to achieve results that have long been out of reach. They managed to reach the G-spot where the brain stimulator can make a major difference for patients with depression.
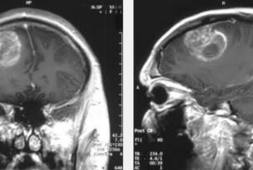
This deep brain stimulation (DBS) succeeded in metabolic brain changes over 12 months that followed the implantation of the device. These results make it a very strong therapy potential for people that tend to be treatment-resistant for their depression, explains the new study.
Former neurosurgery resident at UT-Houston, current fellow with the University of Toronto, and first author Christopher Conner, MD, PhD, said “This is something that people have been trying to do for a long time, but we have not always been very successful with using DBS for psychiatric illnesses.”
He added, “But this PET study shows that we’re altering how the brain is functioning long term and we are starting to change the way brain starts to organize itself and starts to process information and data.”
DBS has actually been used for many years to treat patients that suffer from such movement disorders as Parkinson’s disease, dystonia, and tremor, but it has also been studied to be a possible treatment for people with treatment-resistant depression.
During DBS treatment, electrodes are implanted into particular brain areas, which is where they develop electrical impulses to alter or affect brain activity. But, the challenges with this is finding which part of the brain actually needs to be targeted to treat depression for the long-term.
These new methods target the ‘superolateral branch of the medial forebrain bundle (MFB), which is linked to reward and motivation.’
According to Conner, “We targeted a bundle of fibers that leave this small area in the brainstem to travel to other areas throughout the brain. The PET scans indicated that this small target area has very diffuse downstream effects. It’s not one single effect because there’s not one single area of the brain linked to depression. The whole brain needs to be changed and through this one small target, that’s what we were able to do.”
Before the DBS procedure was performed on the 10 patients that joined the study, the researchers performed initial PET scans in order to get a baseline image. Then, they performed additional PET scans at both six and 12 months to assess any changes after their treatment. From the 10 patients, 8 of them showed a response.
Professor in the Department of Psychiatry and Behavioral Sciences at McGovern Medical School, and co-author João de Quevedo, MD, PhD, said, “A responder to the treatment means that your depression potentially decreases at least 50%; you’re feeling much better. So, for patients with severe chronic treatment-resistant depression, decreasing our symptoms by half is a lot.”
“It’s the difference between being disabled to being able to do something. Correlating with the PET image changes, our patients reported that their depression lessened after the treatment,” de Quevedo added.
If you’d like to see more on the study, De Quevedo, who happens to be the director of the Treatment-Resistant Depression Program, published the paper in the journal, Molecular Psychiatry, with co-authors Dr. Jair Soares, MD and Albert J. Fenoy, MD.