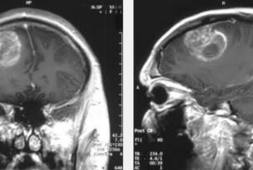
Multiple sclerosis (MS) is a debilitating and life-long disease that affects around 2.3 million people around the world. In the United States, a study found that around 1 million Americans aged 18 are living with an MS diagnosis.
Of the people that have been diagnosed with MS, the majority have initially been diagnosed with relapsing-remitting MS, which means that they will experience periods of acute symptoms. This is called exacerbations or relapses, which normally tend to be followed by periods of less acute or minimal symptoms, known as remissions.As explained by neurologist at the Mellen Center for Multiple Sclerosis at Cleveland Clinic in Ohio, Devon Conway, MD, “When a new neurological symptoms develops in multiple sclerosis, one that isn’t related to an infection and lasts for more than 24 hours, it is considered to be an MS relapse.”
While relapses are caused by inflammation in the central nervous system, remissions – on the other hand – happen when the inflammation dies down. Although not every episode of symptoms getting worse in MS are considered a relapse. According to the Multiple Sclerosis Association of America, when old symptoms reappear and subside within a 24-hour period, such episodes are referred to as pseudorelapse or pseudoexacerbation.
As explained by neurologist and associate professor with the Loyola University Health System in Illinois, Matthew McCoyd, MD, although the cause of a relapse or pseudoexacerbation isn’t always easily identifiable, both have some common triggers.
Here are 4 Common Triggers for MS Symptom Flares and Tips to Avoid Them
1. Stress Can Impact MS
Neurologist at the Mellen Center for Multiple Sclerosis at Cleveland Clinic, Robert Fox, “I don’t know of a single medical condition that is not adversely affected by stress, and there is evidence that stress can worsen the symptoms and the disease of MS.”
One meta-analysis that was published in the Health Psychology Open looked at the way stress impacted MS, finding evidence that stress can be associated with these relapses. The study authors also found that stress and MS relapses can possibly have a bidirectional relationship too, which means that stress can contribute to the development of a relapse, while an MS relapse can also cause stress to occur.
Meanwhile, some of the studies that were part of the meta-analysis showed how accumulated stress or the presence of a number of stressful situations also increased the risk of a relapse as compared to just one stressful event. At the same time, chronic stress that lasted longer than 48 hours has a bigger effect on MS than acute stress.
Dr. Fox shared, “Patients can dismiss stress, but it’s another condition, like high blood pressure or diabetes or obesity; it can impact all aspects of your health and it should be attended to.”
In this light, the National MS Society recommends that a number of strategies to help manage stress such as not doing things you don’t have the energy to do, or asking for help during the times that you need it. Other suggestions are practicing relaxation techniques like yoga, meditation, and deep breathing.
2. A Lack of Sleep Can Worsen MS Symptoms
For patients suffering from MS, they often find themselves struggling to get a good nigh sleep due to temperature dysregulation issues, restless legs, and urinary and bowel symptoms that are some symptoms of MS, making it harder to combat the other stressors that come with having MS. Dr. Conway says, “Most people with MS have a lower reserve of energy,” which lack of sleep can worsen.
Other consequences that come with poor sleep and MS are increased fatigue, pain, anxiety, and problems with coordination. In addition, the Sleep Foundation also shares that people suffering from MS will also more likely to have sleep-disordered breathing, insomnia, narcolepsy, and REM sleep behavior disorder.
According to neurologist Dr. Scott Ireland Otallah, who specializes in MS, shares that if a sleep disorder is suspected, by getting a diagnosis and proper treatment can reduce the relapse likelihood. Other tips include doing lifestyle modifications like keeping a regular waking and bedtime routine, drinking less fluid before going to bed, and limiting alcohol consumption before sleep are also ways to help lessen relapses.
3. Some Common Infections May Cause Pseudoexacerbations and Lead to Relapses
Dr. Otallah explains that there are some infections that can cause MS symptoms to flare, more so when the infection include a fever.
Conway adds, “Urinary tract infections (UTIs) are common causes, because some people with MS have reduced bladder function.” He also says that any type of infection that can weaken the immune system, such as the flu or a cold can also cause a flare.
While technically, a real MS relapse is considered ‘any new or acutely worsening neurological symptoms that are not related to an infection, fever, or other stresses,’ while lasting more than 24 hours, then worsening MS symptoms that happen during a UTI or other type of infection could be a pseuoexacerbation.
But, a review that was published in Frontier in Immunology shared how infections tend to be associated with relapses as well, while some research shows that relapse occurs in an estimated 30 percent of people with MS after having an upper-respiratory infection.
Shared by the National MS Society, some tips to prevent these types of infections to lessen the chances of subsequent relapses are to get the influenza and other types of vaccines to reduce the risk of infections.
4. Common Cause of Pseudoexacerbations is the Summer Heat
One common trigger for MS pseudoexacerbations is increased body heat. In fact, Dr. McCoyd even notes that “in the old days, a hot-bath reset was one of the ways doctors diagnosed MS.” They would immerse the person suspected to have MS in hot water, and if their neurological symptoms seemed to worsen, it was considered evidence that the patient had MS.
Dr. Otallah also said that ‘heat causes the appearance or worsening MS symptoms in areas that have been impacted by previous relapses.’
He says, “So if a person has an area previously affected by demyelination — for example, say, a person had numbness on the left side for a couple of weeks two years ago — even though they’ve recovered from that attack, if they get overheated by being out on a hot day for a long time, their left side might start to feel numb.”
Moreover, Otallah adds that it doesn’t take much to make the old MS symptoms appear. Just a slight elevation of the body temperature – like just half a degree or more – can make them come out.
When an MS patient has temporary worsening of neurological function caused by their core temperature increasing is called Uhthoff’s phenomenon. Usually, the symptoms go away by getting short period of rest, using active cooling methods, and removing heat stressors can help. Dr. Otallah shares, “Getting into air-conditioning, taking a cool shower, or wearing a vest filled with cooled water usually helps reduce heat symptoms.”
How and When To Treat MS Flares
Notably, not all MS symptoms need to be treated, such as mental fog, fatigue and tingling generally going away on their own when the trigger goes away or the infection is treated.
Yet with more severe MS symptoms that affect one’s ability to function properly or normally, like poor balance, loss of vision, and severe weakness, this could mean that you’re having a relapse where a doctor may recommend steroid treatment to lessen the severity and length of the exacerbation.
Just keep in mind that not all of these symptoms are caused by MS. If you happen to experience any of these symptoms, be sure to speak with your doctor about any concerns you may have as well as what needs to be done, if anything.