Brushing your teeth daily reduces the risk of gum disease, which is associated with various cancers. Research indicates that the oral microbiome in individuals with gum disease may be connected to specific types of cancer.
Vital Ideas to Take Note:
- The mouth hosts the second-largest microbiome in the body, following the gut.
- A specific bacterium that is more prevalent in individuals with gum disease has been associated with colorectal cancer.
- Maintaining a routine of regular brushing and flossing can reduce the risk of gum disease, potentially lowering the risk of colorectal cancer as well.
Could the condition of your oral health, including your mouth, gums, and teeth, affect your chances of developing cancer or influence the aggressiveness of tumor growth? Emerging research suggests a significant correlation between gum disease and an elevated risk of various cancers, particularly colorectal and pancreatic cancer. Gum disease, a group of inflammatory conditions targeting the tissues around the teeth, appears to be a contributing factor.
Colorectal cancer, which affects the colon and rectum, stands as the third leading cause of cancer-related deaths among men and the fourth among women in the United States. While advancements in screening techniques have generally led to a decline in overall rates, there has been a troubling increase in colorectal cancer cases among young adults. This rise is likely due to a combination of factors, such as sedentary lifestyles, higher rates of obesity, and diets rich in processed foods and low in fiber. These lifestyle and dietary choices, alongside the presence of gum disease, may compound the risk, highlighting the importance of maintaining good oral health as part of a comprehensive approach to cancer prevention.
Mouth – the Second Largest Microbiome in the Body
An additional contributing factor to the increase in certain health issues could be a type of bacteria found in the oral microbiome of individuals with gum disease. While the gut microbiome, the largest microbiome in the body, has garnered significant attention, the oral microbiome is the second largest and equally diverse, housing over 700 species of bacteria.
Mingyang Song, ScD, an associate professor of clinical epidemiology and nutrition at Harvard T.H. Chan School of Public Health, explains that the oral microbiome and its bacterial balance play a crucial role in overall health. Dr. Song, who has conducted research on the link between the oral microbiome and colorectal cancer, highlights the importance of maintaining a healthy oral microbiome.
Researchers have identified several key bacteria within the oral microbiome that significantly impact health. One such bacterium is Fusobacterium nucleatum. Typically present in low quantities in the mouth, this bacterium can proliferate under certain conditions, leading to inflammation and gum disease. If gum disease is not addressed, it can progress to more severe conditions, including the destruction of bone and tissue that support the teeth, ultimately resulting in tooth loss.
Gum Disease and Tooth Loss Linked to the Risk
The health of the mouth microbiome has been increasingly recognized for its connection to a variety of systemic diseases, including cancer, obesity, diabetes, heart disease, Alzheimer’s disease, inflammatory bowel disease, rheumatoid arthritis, and metabolic dysfunction–associated steatotic liver disease, according to Song. There’s also a noted relationship between the oral microbiome and certain types of cancer, particularly those of the head and neck, as well as colorectal and pancreatic cancers.
Despite these findings, the scientific community still grapples with understanding the precise role that gum disease and the oral microbiome play in the development of these conditions.
Song was a leading researcher in two pivotal studies exploring the link between cancer and gum disease. The first study revealed that individuals with a history of gum disease faced a 52 percent higher risk of developing stomach cancer compared to those without gum disease. Additionally, the loss of two or more teeth was associated with a 33 percent increased risk of stomach cancer. The study also identified a correlation between gum disease and a heightened risk of esophageal cancer.
In the second study, Song and his team found a significant association between gum disease and an increased risk of colorectal cancer. Individuals with a history of gum disease had a 17 percent higher relative risk of developing serrated polyps, a type of colon polyp that can potentially progress to cancer. Approximately 25 percent of colon cancer cases originate from serrated polyps. Furthermore, the loss of four or more teeth was linked to a 20 percent increased risk of having a serrated polyp.
The research also indicated that a history of gum disease was associated with an 11 percent increased risk of conventional adenomas, another type of colon polyp that, while noncancerous, can eventually become cancerous.
Both studies suggested that disruptions in the oral microbiome could be influenced by factors such as poor oral hygiene, genetics, smoking, diabetes, and obesity. Notably, individuals diagnosed with colorectal cancer exhibited higher rates of transmission of the harmful bacterium Fusobacterium nucleatum from the mouth to the gut compared to healthy individuals.
Imbalances in the Mouth Microbiome May be Culprit Behind Inflammation
How harmful bacteria in the mouth may impact other parts of the body, including the potential link to colorectal cancer, isn’t fully understood. Song suggests that both direct and indirect mechanisms could be involved.
The oral microbes can directly gain access to the other parts of the body, which results to damage and inflammation, he said. “Also, alterations in the oral microbiome can cause systemic inflammation and increase disease risk indirectly.”
How Mouth Bacteria Travels
How do bacteria reach the gastrointestinal tract or bloodstream? According to Floyd Dewhirst, DDS, PhD, an emeritus professor of oral medicine, infection, and immunity at Harvard Medical School in Boston, there are a few pathways. Dr. Dewhirst, who has spent decades researching the mouth microbiome, explains that these routes enable the bacteria to travel to other parts of the body.
“Basically, the fate of almost all the bacteria that live in the mouth is at some point to get swept up by saliva and swallowed,” he said.
According to Dewhirst, bacteria travel through the stomach, and if they withstand the stomach’s acidic environment, they can reach the GI tract.
He also notes that numerous bacteria can cause infections in the periodontal and subgingival pockets—the areas surrounding the teeth under the gum line, especially in individuals with gum disease.
“When you do things like bite into an apple or brush your teeth, a small number of these organisms are able to get into the bloodstream from the vessels that are next to the gum tissue. Most of the time the body is good at finding the small number of bacteria and destroying it, but occasionally, something that’s gotten into the bloodstream can circulate through the body and go somewhere else and start an infection,” Dewhirst said.
He mentions that you can spread bacteria from your mouth by getting saliva on your fingers and then touching your eyes, nose, or any broken skin.
Researchers Spots Deadlier Subspecies of F. Nucleatum
Dewhirst co-authored a groundbreaking study published in Nature in March 2024, which may pave the way for improved methods of identifying and targeting aggressive colon cancers.
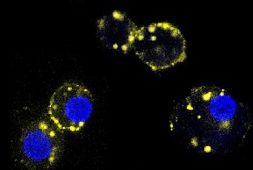
In the study, researchers meticulously compared the genetics of Fusobacterium nucleatum from colorectal tumors with those from healthy oral cavities. They discovered that a particular subspecies of the bacterium, known as Fna, was more prevalent in colorectal tumors. Delving deeper, they identified two distinct variants of Fna. While both variants were present in the mouth, only one variant, Fna C2, was linked to colorectal cancer.
The researchers conducted experiments on mice with inflamed colons, infecting them with the two different types of F. nucleatum. The results were significant: mice infected with Fna C2 developed more tumors compared to those infected with the other variant.
Although the precise mechanism of how these bacteria migrate from the mouth to the colon remains unknown, the study revealed that Fna C2 could survive longer in acidic conditions similar to those in the gut. This suggests that the bacteria might travel directly through the digestive tract, a hypothesis supported by the researchers.
The study emphasized the importance of identifying the specific bacterial lineage associated with colorectal cancer. This knowledge is crucial for developing targeted prevention and treatment strategies to improve patient outcomes.
Bottom Line: Practice Good Oral Hygiene
While it isn’t clear how oral hygiene specifically has an impact on cancer risk, it is known that poor oral hygiene does exacerbate risk of gum disease, Song said. “Practicing oral hygiene is certainly a good practice,” he added.
To minimize the risk of gum disease, it’s important to brush your teeth after meals, floss daily, use mouthwash regularly, and maintain regular dental check-ups with a dentist or periodontist.
Additionally, maintaining a healthy diet and lifestyle, such as regular exercise and abstaining from smoking, contributes to the overall health of the oral microbiome, as noted by Song.