In a groundbreaking human clinical trial, an mRNA cancer vaccine developed at the University of Florida has shown remarkable success in reprogramming patients’ immune systems to aggressively target glioblastoma, the most aggressive and lethal form of brain tumor.
The trial included four adult patients and produced promising results that closely paralleled those observed in a separate study involving 10 pet dogs with brain tumors. The dog owners had consented to their pets’ participation in this innovative research.
This discovery highlights a potential new strategy to engage the immune system in combating treatment-resistant cancers. The vaccine employs a sophisticated version of mRNA technology and lipid nanoparticles, akin to those used in COVID-19 vaccines. However, it incorporates two significant advancements: the use of a patient’s own tumor cells to create a personalized vaccine, and a novel, complex delivery mechanism within the vaccine itself.
These advancements mark a significant leap in cancer treatment, offering hope for more effective therapies against some of the most challenging and resistant forms of cancer.
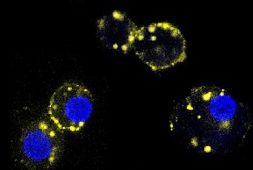
“Instead of us injecting single particles, we’re injecting clusters of particles that are wrapping around each other like onions,” senior author Elias Sayour, M.D., Ph.D., said. He is a UF Health pediatric oncologist who pioneered the development of the new vaccine, which is like other immunotherapies that works to “educate” the immune system that a tumor is considered unknown or foreign.
“These clusters alert the immune system in a much more profound way than single particles would.”
Among the most impressive findings was the rapid onset of a robust immune response against the tumor, remarked Dr. Duane Sayour, principal investigator at the University of Florida’s RNA Engineering Laboratory and an investigator at the McKnight Brain Institute, who spearheaded the multi-institutional research team.
Dr. Sayour emphasized that the new method quickly galvanized the immune system to recognize and attack the glioblastoma cells with remarkable vigor. This swift and potent response underscores the potential of the mRNA vaccine to revolutionize cancer treatment by harnessing the body’s own defenses in a highly targeted manner. The speed and intensity of the immune reaction suggest that this approach could be a game-changer in treating one of the most aggressive and deadly brain tumors, offering new hope for patients facing limited options with current therapies.
“In less than 48 hours, we could see these tumors shifting from what we refer to as ‘cold’—very few immune cells, very silenced immune response—to ‘hot,’ very active immune response,” he said.
“That was very surprising given how quick this happened, and what that told us is we were able to activate the early part of the immune system very rapidly against these cancers, and that’s critical to unlock the later effects of the immune response,” he explained in the video below.
Glioblastoma is one of the most devastating diagnoses, with a median survival rate of approximately 15 months. The current standard of care typically includes surgery, radiation, and a combination of chemotherapy treatments.
A groundbreaking new study, published on May 1 in the journal Cell, presents a novel approach to treating glioblastoma. This report is the culmination of seven years of promising research, which began with preclinical studies in mouse models.
In this study, four patients were treated using an innovative method where RNA was extracted from each patient’s surgically removed tumor. This genetic material was then used to create messenger RNA (mRNA)—a blueprint of the cell’s contents, including tumor cells. The mRNA was amplified and encapsulated in a newly engineered, biocompatible lipid nanoparticle packaging. When reintroduced into the patient’s bloodstream, this mRNA made the tumor cells appear like a dangerous virus, thereby triggering a robust immune response.
This personalized vaccine was tailored to each patient, aiming to maximize the potential of their unique immune system to recognize and attack the tumor cells. This individualized approach could revolutionize the treatment of glioblastoma by leveraging the body’s own defenses in a highly specific and effective manner.
“The demonstration that making an mRNA cancer vaccine in this fashion generates similar and strong responses across mice, pet dogs, and human patients is a really important finding, because oftentimes we don’t know how well the preclinical studies in animals are going to translate into similar responses in patients,” Duane Mitchell, M.D., Ph.D., director of the UF Clinical and Translational Science Institute and a co-author of the research, said. “This is a novel and unique way of delivering the mRNA to generate these really significant and rapid immune responses that we’re seeing across animals and humans.”
Although it is still early in the trial to fully assess the clinical effects of the vaccine, preliminary results are promising. Patients either remained disease-free for longer than expected or survived longer than the typical prognosis. In the parallel study with 10 pet dogs, the median survival was 4.5 months, significantly longer than the usual 30-60 days for dogs with this condition.
The next phase of this research, supported by the Food and Drug Administration and the CureSearch for Children’s Cancer foundation, will be an expanded Phase I clinical trial. This phase will include up to 24 adult and pediatric patients to further validate the initial findings. Once an optimal and safe dosage is established, an estimated 25 children will participate in Phase II.
For the upcoming clinical trial, Dr. Sayour’s lab will collaborate with the multi-institution Pediatric Neuro-Oncology Consortium. This partnership will facilitate the distribution of the immunotherapy treatment to children’s hospitals nationwide. The process involves receiving an individual patient’s tumor, manufacturing the personalized vaccine at the University of Florida, and then sending the customized treatment back to the patient’s medical team. Dr. Sayour, co-leader of the Immuno-Oncology and Microbiome research program at the UF Health Cancer Center, highlighted this coordinated effort as a crucial step in making the treatment accessible to more patients.
“I am hopeful that this could be a new paradigm for how we treat patients, a new platform technology for how we can modulate the immune system,” said Sayour in a UF Health news report made by Michelle Jaffee. “We showed in this paper that you actually can have synergy with other types of immunotherapies, so maybe now we can have a combination approach to unlock those immunotherapies.”