Experts say that there is an increased risk for heart disease as women age, and this happens years after menopause. There was a research that was recently presented in the North American Menopause Society annual meeting and they said that constant hot flashes may be a sign that you’re at an increased risk for suffering from a heart attack or stroke.
Women who are undergoing a menopausal transition will experience hot flashes, which is a kind of “vasomotor symptom.,” this means that they will suddenly feel such intense heat and many of them will break out in sweat. Johns Hopkins Medicine made an estimate and they say that about three-quarters of them will experience these sudden yet brief episodes. While it doesn’t seem like much of a big deal, this can actually affect quality of life, disrupt sleep, increase irritability, and even bring about depression. Hot flash symptoms actually can last for more than seven years as an average, as per the Mayo Clinic. For the more unfortunate few, this can go on for 10 years or even more.
When women reach the menopausal stage, this also means that heart risks go up. That’s because their bodies are no longer able to produce enough estrogen, a hormone that protects the heart. The American Heart Association said that 1 in 3 women has some form of heart disease because they have observed a general increase in heart attacks among women who are in 10 years post-menopausal.
At the North American Menopause Society (NAMS) Annual Meeting that happened in Atlanta last October, Rebecca Thurston, PhD, director of the Women’s Biobehavioral Health Laboratory at the University of Pittsburgh’s School of Public Health gave the audience data on hot flashes and heart disease risk. She also elaborated some guidelines on what women should do and consider to help lower their chances of suffering from heart issues.
“For years, vasomotor symptoms have been regarded as a midlife symptom with few implications for women’s physical health,” said Dr. Thurston. She is now conducting work that’s funded by the National Institutes of Health. “But a growing body of literature is beginning to link these vasomotor symptoms to indicators of cardiovascular disease risk,” she added.
The doctor said that women with frequent or severe hot flashes have higher chances of suffering from conditions that increase the risk of heart problems. Included on the list are high blood pressure, diabetes, high cholesterol, and an even bigger risk of underlying atherosclerosis, which is fat buildup that happens in the arteries, which in turn, can hinder blood flow.
Thurston’s presentation was based from two studies. One of which was the Study of Women’s Health Across the Nation (SWAN). This had more than 3,300 middle-aged women as participants all throughout seven designated research centers across the U.S. The second study was a University of Pittsburgh study published in 2016 in the journal Stroke. The latter had 304 participants that were recruited just locally.
In the second research, Thurston and her collaborators saw how participants with more vasomotor symptoms also experienced more carotid atherosclerosis. This is when blood vessels found in the neck and carry the blood from the heart to the brain become narrow.
Thurston also said that the observations made in the SWAN study and current research that came from different parts of the globe also indicated that hot flashes that were reported were linked to atherosclerosis. It also showed how around one-third of the women seem to experience frequent more vasomotor symptoms that have an impact on heart health.
Findings that came from the SWAN study also exhibited how those who experience more frequent vasomotor symptoms were at 50 to 77 percent greater risk for heart disease. Those who were between the ages 42 and 52 years old at beginning of the study were monitored for up to 22 years. These were capped off with 16 follow-up visits. From the beginning and until each follow-up visit, they were given a standard questionnaire. They were asked to report how often they had vasomotor symptoms such as hot flashes and night sweats in the last two weeks. Some answered that they saw this for six or more days or one to five days. The others also experienced no symptoms.
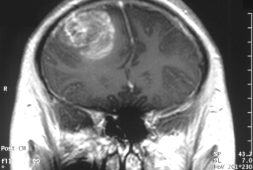
Thurston was also part of another research that looked deeper into the role menopausal symptoms and how these have a part of brain health such as small vessel disease in the brain. One study published in 2016 in the journal Menopause and this may have come across a probable link between hot flashes and white matter hyperintensities. The said hyperintensities are areas of the brain that show up as bright, high signal intensities on MRIs. These are said to be because of chronic ischemia, which is a blood supply deficiency. This lack of blood flow to the brain could bring about a stroke. Still, the authors of the study said that more investigation is needed and mechanisms that connect hot flashes to white matter hyperintensities haven’t been fully clarified just yet.
“There’s essentially a coalescing of information from around the globe that points to the importance of these vasomotor symptoms in women’s cardiovascular health,” said Thurston. “I’ve been struck by how consistently we see this association.”
While some proof has been shown to establish links between frequent and severe flashes and greater heart risk, Thurston and her team of other researchers still are unclear with how to treat these menopausal symptoms to improve heart health. Further research and studies will be needed so that these experts can look into factors such as inflammation, clotting, and hormone changes and how these play a part.
For women undergoing frequent hot flashes, Thurston said that they need to seek treatment with a gynecologist, a primary care provider, or a nurse practitioner. Essentially, they need to go to someone who is trained in menopause care. She said that women need to seriously consider their lifestyle and health habits. “If you’re smoking, now is the time to stop,” she advised. “If you’re having trouble with weight management, get some support for that.”
The American Heart Association also said that women need to get their cholesterol checked every five years, blood pressure every two years, blood sugar levels every three years, and body mass index in each doctor’s visit. Also, they need to get least 150 minutes of physical activity each week so that they can lower their risk of heart disease. They also need to follow a heart-healthy diet.
“During midlife, many things change dynamically for women,” said Thurston. Hence, they need to take control of their lifestyle to avoid further problems. However, she also said that they need not to be too worried about these potential health issues.
“It’s stressful enough to be going through menopause and having lots of these vasomotor symptoms,” said Thurston. “So get your basic vasomotor symptoms treated if they’re really causing you suffering, and make sure you’re on top of your cardiovascular health.”
She also encourages women out there to make their health a priority because many of them worry about others before they even think about themselves. “While that’s a very loving thing to do, prioritizing your own health is critical as well,” she said.