A new case study was done at the University of California in San Francisco (UCSF) suggesting that ‘adapting deep brain stimulation to a patient’s individual needs’ could temporarily relieve depression symptoms.
The study authors discovered that by stimulating three particular brain areas, it could aid in producing calm, reactivate energy levels, or awaken pleasure in patients suffering from depression. This response to the brain stimulation also depended on an intricate interaction among a patient’s mood state, symptoms, and the site of the brain stimulation.
Researchers share that it was in electrically stimulating three different areas in a patient’s brain that worked with three particular symptoms of depression, which are reducing anxiety, boosting energy levels, and restoring pleasure in everyday activities.
One such patient, a 36-year old female, suffered from repeated episodes of severe, treatment-resistant depression since she was a child. Just a few seconds of brain stimulation resulted in ‘a sense of pleasure in life.’
She explained, “Every time they stimulated, I felt like, I’m my old self, I could go bac to work, I could do the things I wasn’t to do with my life.”
The researchers from UCSF that developed this specialized and personalized form of deep brain stimulation (DBS) expanded their clinical trial by including an additional 12 patients under the same condition. Their initial findings were reported in a study paper that came out in Nature Medicine.
The Centers for Disease and Prevention (CDC) states that back in 2019, 4.7% of the United States adult population claimed that they regularly had bouts of depression.
With that, another study shares that at least 1 in 3 patients that are diagnosed with depression are actually resistant to therapy, which means that they don’t respond to psychotherapy or antidepressant drugs. Although a number of these patients can benefit from electroconvulsive therapy, because of the stigma surrounding it, as well as the potential side effects of this type of treatment, they choose not to try it.
Deep Brain Stimulation (DBS)
DBS, or deep brain stimulation, gained popularity in 2003 as an alternative method to electronically stimulate particular areas in the brains of depressed patient’s that are treatment-resistant.
But despite its popularity, the results of the clinical trial have been varied. One example from a 2017 study focused on a single area for brain stimulation, which was the subcallosal cingulate. The study found that although DBS was safe, it was not substantially better than the “sham” DBS at lessening depression. The study authors have suggested that in future research, they will explore other electrode placement sites.
These results also had the UCSF researchers pondering whether mapping each patient’s unique brain activity before targeting the stimulation to specific areas of the brain could actually improve the outcome of treatment. This particular approach has been proven in some patients suffering from Parkinson’s disease and epilepsy.
According to assistant professor in the Department of Psychiatry and Behavioral Sciences at UCSF and corresponding author of the new study, Dr. Katherine Scangos, “The brain, like the heart, is an electrical organ, and there is a growing acceptance in the field that the faulty brain networks that cause depression – just like epilepsy or Parkinson’s disease – could be shifted into a healthier state by targeted stimulation.”
She added, “We know depression affects different people in very different ways, but the idea of mapping out individualized sites for neuromodulation that match a patient’s particular symptoms has not been well explored.”
Another co-senior author of this new study, Dr. Edward Chang, had previous work that showed this approach worked well for patient’s diagnosed with depression at the UCSF Epilepsy Center. These patients already have electrode arrays implanted in their brains which allowed surgeons to map the location of seizures before opting for epilepsy surgery.
Yet, the question still remains whether this brain-mapping approach will also work for those patients that are diagnosed with depression and nothing else.
Ongoing Clinical Trial
During the first phase of the new trial, which is called PRESIDO, the UCSF research team will identify which networks improve when stimulated in every patient’s brain. The goal of the study is ‘to program neuromodulation devices to respond in real-time to warning signs in these networks with targeted stimulation that restores balance to the patient’s brain circuits.’
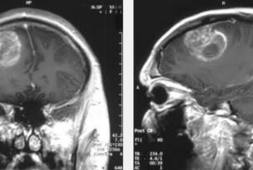
In the study paper, the research team talk about how they inserted 10 electrodes into the brain of their 36-year old female participant, who also happened to be their very first enrolled patient in the trial. Then over the next 10 days, they mapped the effects of mild electrical stimulation over the various brain regions where previous studies proposed moods were possibly affected.
After an assessment by psychiatrists and a set of standard questionnaires, the research team also found that 90-second stimulation of three specific sites quickly and dependably produce three distinct and positive emotional states.
Meanwhile, researchers also managed to stimulate a region that involved processing reward, which is known the ventral capsule or ventral striatum. When this happened, the patient shared that they felt “tingles of pleasure.”
Then, when they stimulated the subgenual cingulate, which aids in regulating one’s mood, the patient claimed that she felt a “neutral alertness […] less cotton and cobwebs.”
By stimulating each of the three sites one after another between 3 to 10 minutes, it improved the patient’s symptoms in a variety of ways, depending on what her emotional state was at the time of treatment. For instance, when she was anxious, by stimulating the orbitofrontal cortex, it had a calming effect. But, if the participant was feeling apathetic, stimulating the same brain site made her mood worse or made her feel sleepy. In contrast to this, when stimulating the two other areas heightened her energy levels and arousal.
Glee and Happiness
The 36-year old patient remembers the transformation that happened during her first exploratory phase of her DBS treatment.
“I’ve tried literally everything, and for the first few days, I was a little worried that this wasn’t going to work […] But then when they found the right spot, it was like the Pillsbury Doughboy when he gets poked in the tummy and has that involuntary giggle. I hadn’t really laughed at anything for maybe 5 years, but I suddenly felt a genuine sense of glee and happiness, and the world went from shades of dark gray to just – grinning.”
The patient’s symptoms improved considerably during the course of the 10-day study. The research team then implanted a long-term neuromodulation device that could stimulate her brain at the right time and at the right place, depending on the mood she was in.
According to the PRESIDIO trial, the researchers reprogrammed the device to perceive what the brain signature is in a depressed mood. It then uses mild to undetectable stimulation to the formerly identified brain areas in order to counter effect the mood changes.
Since the device was activated in August of 2020, the patient shared that she has been almost completely depression symptom-free since.
In order to assess whether the improvements on the patient are because of a placebo effect, the next phase of the trial which will be across one year, the research team will include two six-week periods when they will switch off the device and the patient won’t know when it will be on or off.