You might have heard experts say that the gut is the body’s second brain. And within the gut, there’s an entire community of bacteria living there, which play a gigantic role when it comes to a number of human health conditions, one of which is inflammatory bowel disease, or IBD. Ask anyone that’s inflicted with IBD and they’ll tell you that it’s no fun, especially when patients are hit with symptoms such as cramping, swelling, diarrhea, weight loss and fatigue.
Recently, researchers have managed to develop a multifunctional “designer” probiotic that helps treat the many health issues that come with having IBD. Since testing it on mice, it has helped lessen inflammation, reversed some damage to the tissues, and also aided in the restoration of gut microbiome in the mouse model.
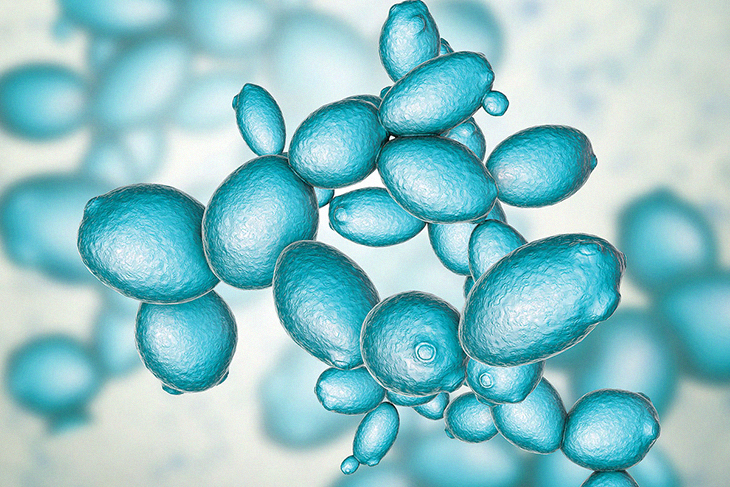
Amazingly, the probiotic happens to be created from the same type or species of yeast that’s used to make beer, by using CRISPR-Cas9, a gene-editing technology. While they recently published their preclinical study, the research team hopes to conduct more safety studies before they head into using the probiotic in human trials.
While the human gut is said to be a host of fungi, bacteria and loads of other microbes in order to help maintain the delicate balance within, it’s harmony hugely influences one’s overall health. What is known as dysbiosis, which is the described by ScienceDirect ‘as a reduction in microbial diversity and a combination of the loss of beneficial bacteria,’ scientists have found that chronic health conditions just like IBD are linked to it.
But the question is, what if there was some sort of supplement that could actually sense disturbances in the microbiome and restore balance to them in order to treat such chronic diseases? This is what the scientists from the Brigham and Women’s Hospital in Boston, MA are saying they have made. They created a “designer” probiotic which they claim can do exactly that.
According to their new study published in Nature Medicine, the researchers created a genetically engineered yeast that responds to inflammation, which when used on the mice, has successfully relieved their symptoms of IBD.
The Link Between IBD and Gut Microbiome
The term IBD is actually an umbrella term, which means that it is used to explain a variety of conditions, yet most of them are characterized by relentless inflammation of the gastrointestinal tract. Two of the most common types of IBD are ulcerative colitis and Crohn’s disease.
Back in 2015, the Centers for Disease Control and Prevention (CDC) reported that around 3 million adults within the United States were diagnosed with IBD. Some of the most common symptoms are abdominal pain, diarrhea, bloody stools, unexplained weight loss and fatigue.
Meanwhile, older studies found that patients with IBD normally have unbalanced gut microbiome, which means there is a lower microbiome diversity overall, and more species of bacteria that causes inflammation. Scientists are under the impression that probiotics actually help restore the balance of the gut while lessening the inflammation.
Yet, the probiotics are available on the market ‘have been optimized through evolution in a healthy gut.’ In the new study, the scientists believe that in order to best handle IBD, the probiotic would need to have a number of functions such as stopping any inflammation, reversing the damage to the tissues and restoring balance to gut bacteria.
Yeast Robots
One of the investigators at the Brigham and Women’s Hospital, Dr. Francisco Quintana, alongside his colleagues, wanted to create a probiotic that had the ability to address and fix all these health issues.
He explained to Medical News Today, “What we wanted to […] do was to use a platform that would allow us to manipulate the new response in a very specific way, when and where needed. And that led us not to any probiotic but actually to yeast.”
The term “yeast robots”, which was affectionately created by the science team, shares how the probiotics were created from the yeast species Saccharomyces cerevisiae, which is the same type of yeast that’s used in baking, and to make beer and wine.
While it’s known to live naturally within the human gut as a part of the healthy microbiome, it is not a commonly used as a probiotic.
What Dr. Quintana and his team did was use the gene-editing technology CRISPR-Cas9 in order to introduce a gene that is normally activated in the gut via inflammation.
What happens is that when the yeast becomes aware of the inflammation, it ends up secreting an enzyme that ‘degrades inflammatory molecules called extracellular adenosine triphosphate (eATP)’ which results in reduced inflammation.
This engineered yeast generates various amounts of the enzyme depending on the amount of inflammatory signals that are present in the gut. This way, the yeast becomes “self-tuning,” which means that it can give a ‘highly localized response to specific sites of inflammation within the gut.’
Dr. Quintana shares, “It’s the idea of taking individualized medicine to the extreme. This is not only for a specific patient but specifically for each micropiece of tissue.”
Testing the Mouse Models
The research team tested their “designer” probiotics on mice that had many different kinds of IBD. After the mice were orally given the engineered yeast, the researchers saw that the mice had lower expression of genes that boost the inflammation in the colon.
Because of this, it led to ‘suppressed intestinal inflammation and reduced fibrosis,’ which is normally when the gut lining ends up getting thickened and scarred and can eventually cause blockages in the intestines.
The scientists also observed that for some cases, the engineered probiotics worked just as well in effectivity as some medications that are used to treat people with IBD, like tumor necrosis factor (TNF)-blocking antibodies.
Dr. Quintana also shared with MNT, “In some models, they perform literally as well. And in some of the models we use, the yeast actually outperformed, for example, TNF-blocking antibodies.”
But Dr. Quintana and his team also explain that before the engineered probiotic can be used in humans, they will need to do more safety studies and engaging large-scale clinical trials. The scientists further plan to refine the yeast more so that it can target speeding up tissue repair.
Dr. Quintana also explained that the hope of the probiotic could go further than just dealing with the gut. He explained, “We’re using the gut as a window to really target inflammation in many other tissues.” In fact, his team has even looked into the role of inflammation in the brain in patients suffering from multiple sclerosis, and they hope to further look into the way these genetically engineered yeast robots could possibly offer new types of treatment.
He adds, “If we think in terms of software and hardware, these are hardware, where you can incorporate a code, which is a piece of software. That will allow you to target not only different aspects of IBD but also different inflammatory conditions.”



