Deep sleep is a must. This is when waste products are cleaned from the brain. Included here is the toxic protein called beta-amyloid, which is what’s implicated in Alzheimer’s disease. As researchers have een, those who have disrupted breathing during sleep end up snoring. This is what’s called sleep apnea, and those who suffer from it may not get enough deep sleep.
What happens when you lack sleep? You’ll notice reduced alertness and poor cognitive performance in the person. And now, experts have associated this with an increased risk for Alzheimer’s disease. In fact, a pilot study has been made and the findings suggest that a device that restores healthy breathing in sleep can also improve cognitive performance in those who suffer from the early stages of Alzheimer’s disease.
What Happens During Sleep
The brain flushes away waste through a network of channels known as the glymphatic system. This happens during deep sleep. The waste products are toxic proteins such as alpha-synuclein and beta-amyloid. As mentioned previously, these are implicated in Parkinson’s disease and Alzheimer’s disease, respectively.
However, there’s also a condition that health experts call sleep-disordered breathing (SDB). This is when the upper airway of the respiratory tract repeatedly collapses. This has the ability to disrupt the cleansing process that happens during sleep. The mild case causes snoring, but the more severe form known as obstructive sleep apnea (OSA) stops respiration in its tracts for several seconds at a time. The worst part is that respiration halts completely.
Sleep apnea prevents people who suffer from it from getting the rest they need. They feel tired and fatigued during waking hours, they experience difficulty concentrating, and they will experience problems with memory. That’s because OSA prevents the brain from entering into the deepest phase of sleep, or what they call slow wave sleep. During this time, the brain’s waste disposal system is doing its hardest work.
A Buildup of Toxic Proteins
Studies have connected OSA in the development of Alzheimer’s and Parkinson’s disease. They say that this may possibly be because of the accumulated toxic proteins that weren’t cleaned. “There are a number of studies showing that sleep apnea increases one’s risk of developing Alzheimer’s disease,” explained Jean-Paul Wiegand, Ph.D., preclinical program manager at the Center for Innovation in Brain Science at the University of Arizona Health Sciences in Tucson.
He spoke to Medical News Today and said that there is also proof that sleep disturbance can be an early symptom of Alzheimer’s. He spoke, “Sleep apnea is a multifaceted contributing factor to [Alzheimer’s disease], as it [affects both] sleep quality — and, subsequently, the long-term memory consolidation that occurs during restful sleep, as well as amyloid clearance — and cardiovascular health.”
There is a study made in 2014 that reported how common treatment for sleep apnea known as continuous positive airway pressure can stall cognitive decline in its tracks, thus improving the early symptoms of Alzheimer’s disease. Then, a new study also found how another treatment called myTAP can improve respiration patterns during sleep, especially in those who snore. There were clues made in this small pilot study. The researchers saw that the treatment may improve cognitive performance in those with mild cognitive impairment and the said disease.
Reduced Snoring
The myTAP is a customized oral appliance. It was designed to snap into place over the teeth. What the device does is push the lower jaw slightly forward. This will ease the breathing through the nose and thus, reduce snoring. Health experts believe that breathing through the nose the brain activity that is very much important when entering deep, or slow wave, sleep.
A team of researchers at the Center for BrainHealth, which is part of the University of Texas at Dallas and Texas A&M University, conducted a study with those who snore. The participants were aged 50 to 85 years old. Of those who were at the start of the research, 14 were cognitively healthy, 14 had mild cognitive impairment, and 9 suffered from Alzheimer’s disease.
For them to get the baseline data, the researchers asked these volunteers to sleep as normal at home. They were asked to bring portable recorders with them in order to measure their breathing rate, heart rate, and snoring. During the daytime, the researchers made assessments on their memory, executive function, and attention.
The scientists made some interesting discoveries. The respiration rate, or the number of breaths per minute, that happened during sleep fluctuated significantly more when they compared those who were cognitively healthy to those who suffered from Alzheimer’s disease. Some of them were then asked to use the myTAP device during bedtime for 4 weeks straight. Of these, 5 of them were cognitively healthy, 7 suffered from mild cognitive impairment, and 6 suffered from Alzheimer’s.
After the four weeks was completed, all of them were observed to have a lower maximum breathing rate. This meant that their sleep quality had very much improved. The improvement was also seen most in those with Alzheimer’s, then in those with mild cognitive impairment, then lastly, in those who were cognitively healthy.
The clinicians also saw improvements in breathing rate fluctuation. It’s good to note, however, that the results seen were not considered statistically significant.
The researchers also think that if larger studies will confirm their results, their device could help health professionals when they need to diagnose mild cognitive impairment and Alzheimer’s disease, specifically in those who snore.
“We saw three distinct patterns amongst the groups of people, meaning we can look for a breathing pattern that might predispose individuals to having dementia,” shared Emet Schneiderman, Ph.D., one of the researchers involved and a professor in the Department of Biomedical Sciences at Texas A&M University College of Dentistry.
Cognitive Improvements Seen
After 4 weeks of treatment, the executive and memory functioning of participants improved significantly especially in those with mild cognitive impairment. They have also seen improvements in some of those with Alzheimer’s. Generally, the study was unfortunately too small to identify any statistically significant improvements and changes in cognitive performance in those living with disease.
Still, the researchers believe that a longer period of treatment may be required for them to conclude that they have seen substantial improvements. “If we can make significant changes for individuals with mild cognitive impairment, we can slow the onset of Alzheimer’s disease,” shared Dr. Namrata Das, Ph.D., MPH, who is a postdoctoral fellow at McLean Hospital, Harvard Medical School, in Belmont, MA., and another researcher on the team.
The findings and details of the study appear in the journal Geriatrics.
More Work Conducted is Needed
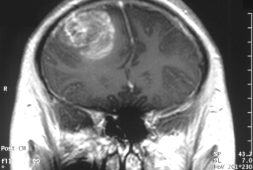
The researchers are looking for further funding for a follow-up study. This time, they will incorporate the use of MRI in order to detect possible structural changes happening in the brain with the treatment they’ll apply. This research will also look into possible changes in the blood levels of beta-amyloid and tau, which, as we said, are the toxic proteins linked to Alzheimer’s.
“We are in the process of applying to [the National Institute on Aging] for a larger study with submission in February 2022 and will integrate MRI scans and blood tests for amyloid beta and tau proteins,” ssenior author Preetam Schramm, Ph.D., from Texas A&M University College of Dentistry, said in an email exchange with MNT.
“Treating poor sleep will serve to rescue immediate behavioral deficits of impaired memory consolidation at night, but it will take time to observe whether it alleviates amyloid buildup,” said Dr. Wiegand. He also concluded, “I believe this study is a step in the right direction to attack one of the most pervasive and understudied contributing factors to [Alzheimer’s disease]. Applied early, the effect could be cumulatively beneficial.”
The doctor also approached the study cautiously. He said that a combination of treatments may be needed to look into all the underlying causes of Alzheimer’s disease in the brain.